Cystic masses
Ignore, Follow, Excise
David S. Hartman, MD and Ileana Chesaru, MD.
From the Department of Radiology, Milton S. Hershey Medical Center, Penn State University School of Medicine, U.S.A and the Westeinde hospital the Hague, the Netherlands.
Publicationdate
This article is based on a presentation given by David Hartman and adapted for the Radiology Assistant by Ileana Chesaru.
In the menubar in the upper left, you will find interactive cases.
Introduction
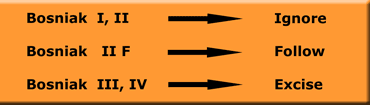
Bosniak Classification of Renal Cystic Disease
The Bosniak classification was described in 1986.
This classification helps the radiologist to categorize each cystic renal mass as "nonsurgical" (ie, benign in category 1 and 2) or as "surgical" (ie, requiring surgery in category 3 and 4).
After the original description, it became obvious that there were some category II cysts that were slightly more complicated than most category II lesions, but not complicated enough to place them in category III.
For that reason, a category IIF (F for follow-up) was introduced in 1993.
Category I (simple cysts), Category II (mildly complicated benign cysts), and Category IV (cystic neoplasms) are easy to diagnose.
Their clinical management is straightforward, with surgery indicated for category IV masses while category I and II masses can be dismissed as benign.
Category IIF ('F' for follow-up; moderately complicated cystic masses that require follow-up imaging to demonstrate stability and therefore benignity) and Category III masses (indeterminate masses that require surgery in most cases) can be difficult to differentiate and are subject to interobserver variability.
This distinction is essential because their treatment is different.
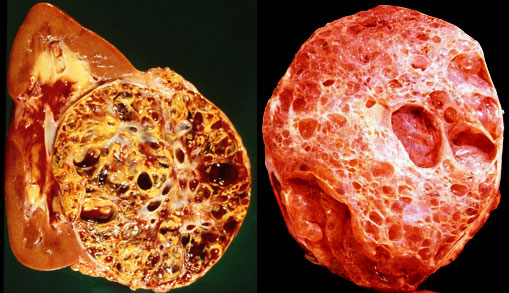
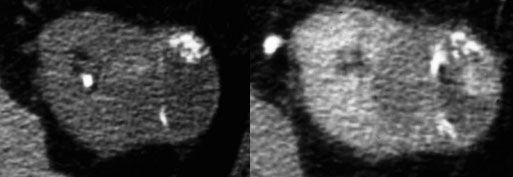
 Even on gross examination a cystic renal cell carcinoma (left) may be indistinguishable from a complicated cyst (right)
Even on gross examination a cystic renal cell carcinoma (left) may be indistinguishable from a complicated cyst (right)
Renal cysts are commonly encountered lesions in daily radiological practice.
Usually these are simple benign cysts, but they can become complicated in case of hemorrhage, infection and ischemia.
When this occurs it can be difficult to differentiate these complicated cysts from cystic renal cell carcinomas (10% of all renal cell carcinomas)
Since the only treatment for renal cell carcinoma is surgery or ablation, we need to recognize these cystic renal cell carcinomas.
Imaging is a reliable means for differentiating benign from malignant cystic lesions.
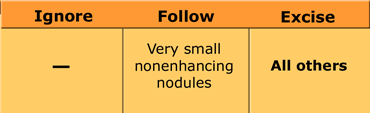
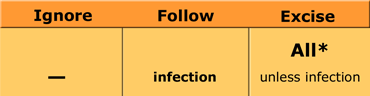
Ignore, Follow or Excise
Renal cysts can be classified according to the Bosniak classification depending on their features.
Type I cysts are simple cysts.
Type II are the minimally complicated cysts.
Type I and II can be ignored.
Type II F are probably benign, but need to be followed.
Type III and IV both are surgical lesions.
Type IV is inevitably malignant and in the type III group about 80-90% turn out to be malignant as well.
In our communication with the clinicians it is important, that we explain the significance of our findings and the meaning of the classification in terms of: Ignore (type I and II), Follow (type IIF) or Excise (type III and IV).
So in this lecture we will only talk about Ignore, Follow or Excise.
For those who want to see the original Bosniak classification, look at the table which is presented at the end of the lecture.
 Differentiation is based upon histologic diagnosis, but Imaging is a reliable means for differentiating benign from malignant cystic lesions
Differentiation is based upon histologic diagnosis, but Imaging is a reliable means for differentiating benign from malignant cystic lesions
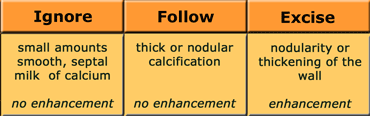
Radiological Interpretation
Although the final differentiation of cystic renal masses is based upon histologic diagnosis, there are imaging findings that tell you that a cyst is not a simple cyst and whether it is probably benign or malignant.
The following imaging features indicate that a cyst is NOT simple:
- Calcification
- Hyperdense / high signal
- Septations
- Multiple locules
- Enhancement
- Nodularity / wall thickening
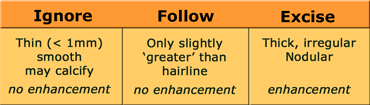
The table on the left summarises these imaging features together with the management consequences: Ignore, Follow or Excise.
When we look at these imaging features, we have to realise, that the most worrisome portion of a cystic mass should be used in deciding appropriate management.
So when the findings are discordant either within one examination or using different radiological examinations, the lesion should be managed based upon the most aggressive imaging findings.
When we look at the table on the left, we can say that we are pretty good with the first 3 parameters (calcification, hyperdens and septations), because we are correct in about 95% of the cases.
The other four are even more easy, because when you have any of these (enhancement, multiloculated, nodularity or wall thickening), the lesion is almost always a surgical lesion.
Regarding follow up, there are no rules at the moment.
One could do a follow up at 6 months and if the lesion is stable then double the follow up time.
We will now discuss all these imaging features in detail.
Calcification
The most important thing is a good description of the type of calcifications.
We can ignore small amounts of calcification that are smooth, septal or if it is milk of calcium, which moves to the lowest point with positional changes.
We have to make sure, that no enhancement (=
All lesions that show enhancement and lesions with wall thickening or nodularity of the wall outside the calcifications should be excised.
We can follow lesions with thick or nodular calcification without any enhancement.
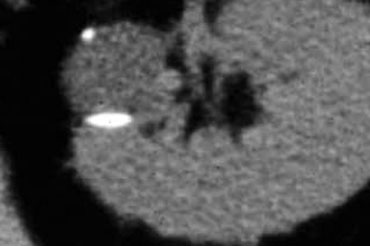
On the left we see a cystic lesion.
There is a small punctate calcification that we can ignore.
On the bottom of the cyst there is a layer of calcium typical for milk of calcium.
This is also a benign calcification that we can ignore.
 LEFT: NECT with a smooth linear calcification and nodular calcification.RIGHT: Enhanced CT shows enhancement ...... Excise
LEFT: NECT with a smooth linear calcification and nodular calcification.RIGHT: Enhanced CT shows enhancement ...... Excise
On the left a patient with nefrolithiasis.
There is also a cystic lesion with linear and nodular calcification .
If there were only these linear calcifications we could ignore the lesion.
In case of nodular calcification we can follow it, if there is no enhancement.
In this case however we see enhancement, so this lesion has to be excised.
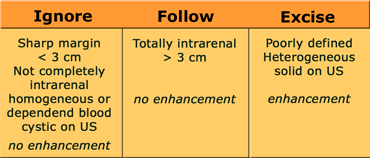
Hyperdense or High signal
On CT hyperdense means: > 20 HU on a NECT
On MRI hyperintense means all that has higher signal intensity than water on a T1 weighted image.
Hyperdensity or hyperintensity usually indicates hemorrhage or high protein content of the cyst.
Ignore all lesion with sharp margins; lesions
On US they have to be clearly cystic
Follow all lesions that are totally intrarenal, because you can not appreciate the wall and follow all lesions > 3 cm, because there is at the moment not much experience with these lesions.
All these lesions must show no enhancement.
Excise all lesions that are poorly defined or heterogenous or show enhancement.
Also when ultrasound shows that the lesion is solid, the lesion should be excised.
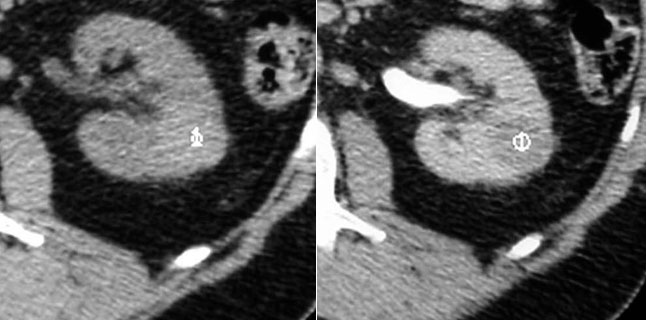
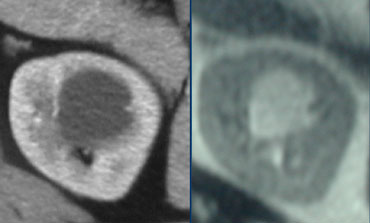
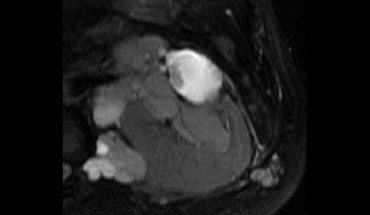
 LEFT: NECT shows a lesion with a density of 27 HU.....IgnoreRIGHT: MRI shows a intrarenal lesion that is hyperintense on T1: higher signal than water...... Follow
LEFT: NECT shows a lesion with a density of 27 HU.....IgnoreRIGHT: MRI shows a intrarenal lesion that is hyperintense on T1: higher signal than water...... Follow
On the left we see a hyperdens cystic lesion on CT and a hyperintense lesion on a T1-weighted MR.
Both lesions have a sharp margin and are homogeneous, although there is some noise in the CT image.
On the enhanced scans (not shown) the lesions didn't show any enhancement.
We therefore can ignore the lesion on the left and we have to follow the lesion on the right, because it is totally intrarenal.
Septations
Ignore thin septations (
Follow all septations that are only slightly 'greater than hairline'. They still have to show no enhancement.
Excise all septations that are thick, irregular or nodular and all septations that show enhancement.
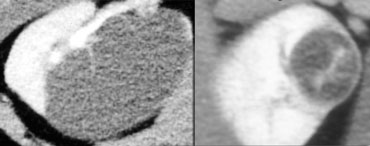
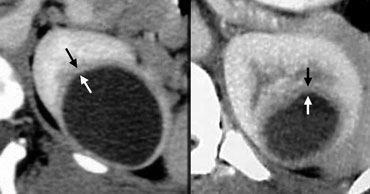
On the left we see 2 cases
There is a cystic lesion with a thin smooth non enhancing septation that we can ignore.
The other case is a thick enhancing septation that has to be excised.
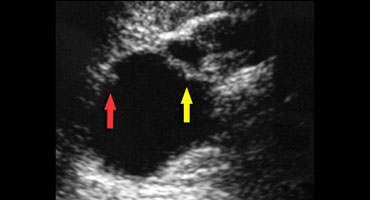
The ultrasound image on the left shows a thick septation.
There is also a nodule in the wall of the cyst.
So we have two reasons to excise this cystic lesion.
Enhancement
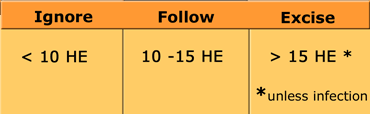
Enhancement is our best predictable sign of malignancy.
So we have to excise all lesions, that clearly show enhancement.
The only exception is infection.
Enhancement is defined as follows: Increase in Hounsfield Units of the mass after contrast injection:
- 10-15 HU = indeterminate
- >15 HU = vascularity
On MR:
>15% = enhancement = surgical
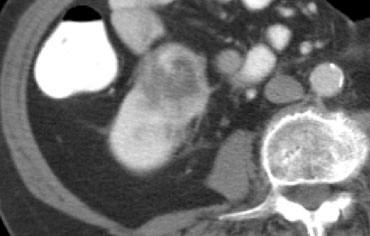
The case on the left doesn't shows much on the NECT.
However when we give contrast we can appreciate a thick wall and we see enhancement both of the wall and of a central area in the medial part of the cystic lesion.
We should never see this in an benign cyst, so this is a surgical lesion.
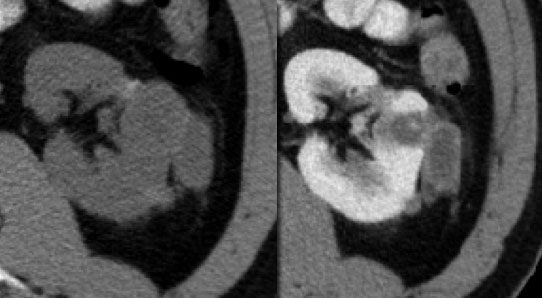
Multiloculated
Masses with three or more septa are not called multiseptated but multiloculated.
All multiloculated lesions should be excised, unless there is clear evidence of infection.
In the adult, the two most common multiloculated masses are MLCN (multilocular cystic nephroma) which is usually benign, but sometimes malignant and MLRCC (multilocular renal cell carcinoma) which is always malignant.
On imaging there is no way that we can separate these two and therefore, all multiloculated masses are surgical (unless infection).
Even the pathologist can not separate the usually benign multilocular cystic nephroma from the malignant multilocular renal cell carcinoma on gross specimen .
The differentiation is based on the histology of the epithelial cells lining these locules.
So all multilocular renal masses have to be excised.
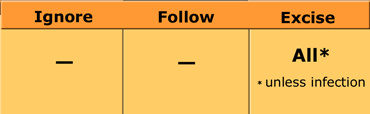
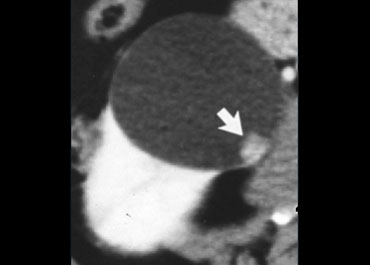
Nodularity
Ignore: none
Follow: only very small nonenhancing nodules, and follow carefully
Excise: all other nodular lesions
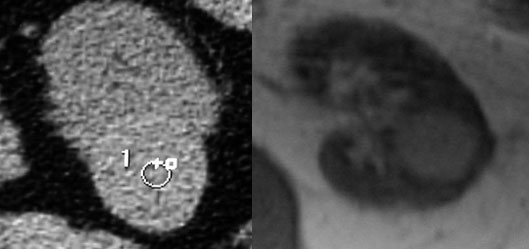
The case on the left shows very small nodules on a CECT and a T2WI.
From all the other images we could tell that they were not enhancing.
So we can probably follow this lesion.
If they start to grow or show any enhancement, then we have to excise the lesion.
On the left an easy case.
There is a big nodule with enhancement, so this lesion has to be excised.
Even if there was no enhancement, the lesion still had to be excised.
The case on the left is a T2WI with Fatsat.
We see multiple nodules so this mass has to be excised.
It doesn't matter whether or not these nodules enhance.
Wall thickening
All lesions with a thickened wall, with or without enhancement, should be excised, unless there is clear evidence of infection.
In these latter cases the lesions should be followed.
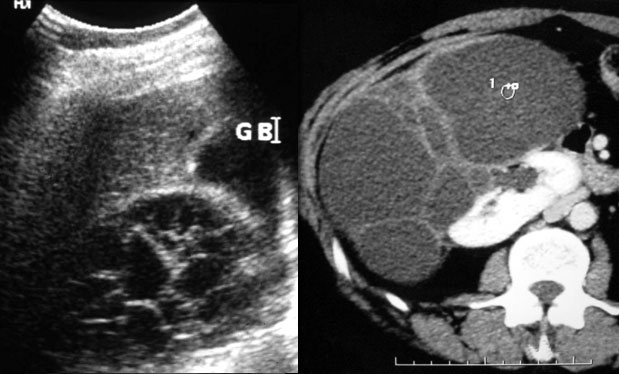
On the left we see two renal lesions that are cystic.
The lesion on the far left clearly shows a thickened wall. This is easy to appreciate because part of the lesion is extrarenal.
The cystic lesion next to it is totally intrarenal, which makes it harder to appreciate, but there is wall tickening.
So both lesions have to be excised, whether there is enhancement of the wall or not.
The only exception would be if there were evident signs of infection.
The cystic lesion on the left is clearly a surgical lesion.
It has a thick irregular wall, it is exophytic and shows enhancement.
Role of Biopsy
In the literature there are different opinions concerning the role of biopsy in renal cystic lesions.
Here we provide Dr Bosniak's opinion.
A different opinion is given by Dr Lang in the artice on CT-guided biopsy of indeterminate renal cystic masses (Bosniak 3 and 2F): accuracy and impact on clinical management (see references)
Dr Bosniak's opinion
Biopsy plays a limited role.
Only in case of clinical suspicion that the mass is inflammatory (pyuria, etc.) or when there is radiological evidence suggesting inflammation (such as perinephric fat stranding), puncture is acceptable.
When the outcome is infection, the lesion can be treated and followed.
Although considered rare, needle track spread of tumor is an 'underestimated risk'.
A core biopsy of the wall of a cystic lesion (benign or malignant) can cause it to rupture and spill its contents into the surrounding tissues.
A negative biopsy result does not rule out malignancy, particularly in cystic lesions that have less bulk of tissue to sample.