COVID-19 Imaging findings
COVID-19 is a viral disease also known as SARS-CoV-2 or severe acute respiratory syndrome coronavirus 2.
The diagnosis is made by a positive PCR test, which is highly specific.
CT has a higher sensitivity but lower specificity and can play a role in the diagnosis and treatment of the disease.
In this article we will describe the role of imaging.
Click here to go to the covid-19-ct-report-template.
Press ctrl+ for larger images and text on a PC or ⌘+ on a Mac.
This can be helpful for scroll-images.
Single images can be enlarged by clicking on them.
Introduction
Clinical Features
COVID-19 usually presents with fever (85%), cough (70%) and shortness of breath (43%), but abdominal and other symptoms are possible and the disease can be asymptomatic.
Overal mortality rate is 2.3% in some series of patients who had a positive test for COVID-19.
Since we do not know the number of people who were infected but not tested for the virus, the actual mortality rate of all the people that are infected is probably much lower.
Illness severity can vary from mild to critical.
- Mild: no symptoms, mild caughing and fever.
- Severe: dyspnea, hypoxia or > 50% lung involvement on imaging.
- Critical: respiratory failure, shock, multi-organ failure.
PCR-test
The PCR-test is very specific, but has a lower sensitivity of 65-95%, which means that the test can be negative even when the patient is infected.
Another problem is, that you have to wait for the test results, which can take more than 24 hours, while CT results are available right away.
Common laboratory findings in COVID-19 are a decreased lymphocyte count and an increased CRP and high-sensitivity C-reactive protein level.
Chest CT
Ground glass
Ground glass (GGO) pattern is the most common finding in COVID-19 infections.
They are usually multifocal, bilateral and peripheral, but in the early phase of the disease the GGO may present as a unifocal lesion, most commonly located in the inferior lobe of the right lung (6).
CT-images of a young male, who had fever for ten days with progressive coughing and shortness of breath.
Saturation at admission was 66%.
The PCR test was positive for COVID-19.
There are widespread bilateral ground-glass opacities with a posterior predominance.
Crazy paving
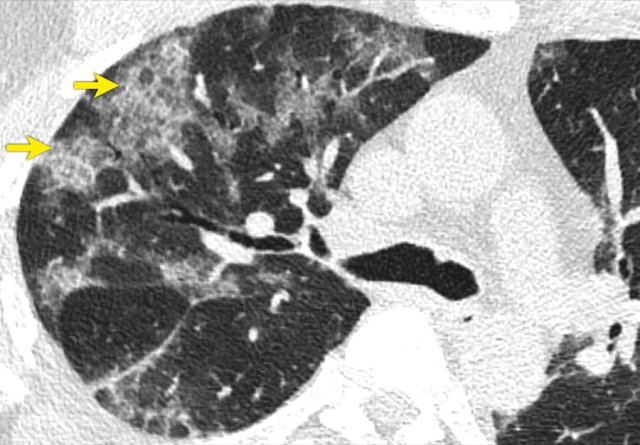
Sometimes there are thickened interlobular and intralobular lines in combination with a ground glass pattern.
This is called crazy paving.
It is believed that this pattern is seen in a somewhat later stage.
Vascular dilatation
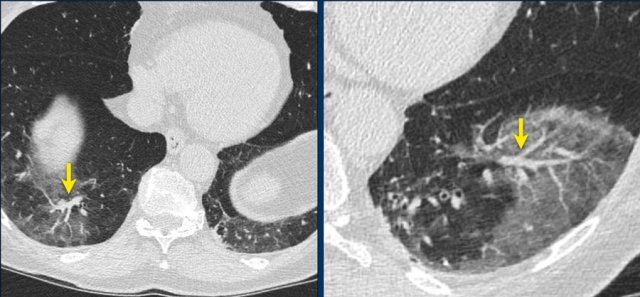
A typical finding in the area of ground glass is widening of the vessels (arrow).
Traction Bronchiectasis
Another common finding in the areas of ground glass is traction bronchiectasis (arrows).
Subpleural bands and Architectural distortion
In some case there is architectural distortion with the formation of subpleural bands.
CT involvement score
The severity of the lung involvement on the CT correlates with the severity of the disease.
Visual assessment
The severity on CT can be estimated by visual assessment.
This is the easiest way to score the severity.
The CT images show a 25% involvement by visual assessment.
Severity score
Another method is by scoring the percentages of each of the five lobes that is involved:
- < 5% involvement
- 5%-25% involvement
- 26%-49% involvement
- 50%-75% involvement
- > 75% involvement.
The total CT score is the sum of the individual lobar scores and can range from 0 (no involvement) to 25 (maximum involvement), when all the five lobes show more than 75% involvement.
Some say that the percentage of lung involvement can be calculated by multiplying the total score times 4.
This however is not true. Suppose that all lobes have a 10% involvement, then this would lead to an overall score of 10, which could lead to the impression that 40% of the lungs are involved.
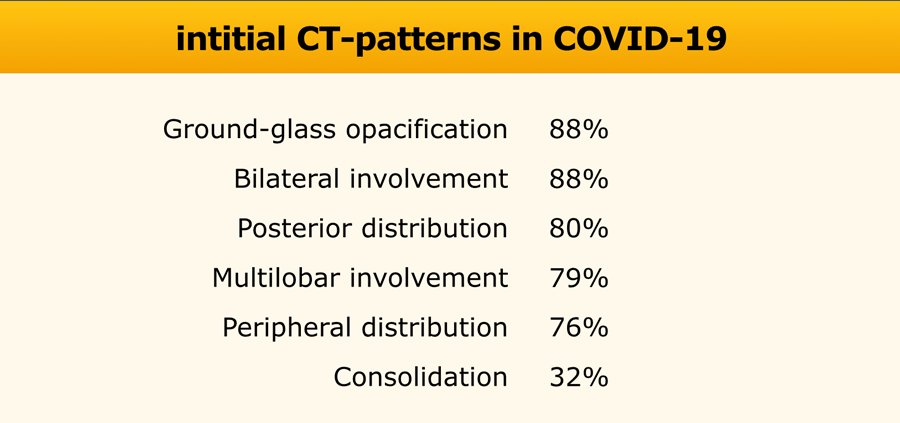
Initial CT-findings
Initial CT-findings in COVID-19 cases include bilateral, multilobar ground glass opacification (GGO) with a peripheral or posterior distribution, mainly in the lower lobes and less frequently in the middle lobe (4).
Consolidation superimposed on GGO as the initial imaging presentation is found in a smaller number of cases, mainly in the elderly population.
Septal thickening, bronchiectasis, pleural thickening, and subpleural involvement are some of the less common findings, mainly in the later stages of the disease.
Pleural effusion, pericardial effusion, lymphadenopathy, cavitation, CT halo sign, and pneumothorax are some of the uncommon but possible findings seen with disease progression.
There is much overlap of the CT-pattern of COVID-19 with other viral pneumonias.
CT-images of a 78 year old male with coughing for 2 weeks and progressive shorteness of breath, who tested positive for COVID-19.
There are bilateral ground-glass opacities with a posterior predominance.
In the right lower lobe there is a consolidation and there is bronchiectasis especially in the left lower lobe.
About 75% of the lungs are involved.
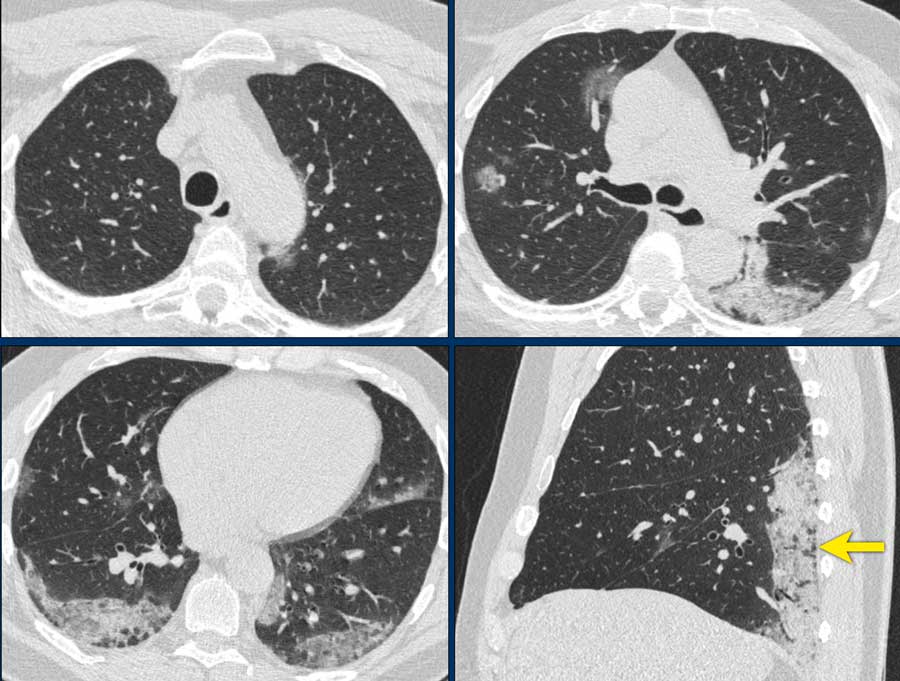
Images of a 59 year old male who had fever for one week with non-productive cough.
The PCR-test was negative.
Because of clinical suspicion a CT was performed which showed some areas of GGO and massive consolidation in the posterior parts of the lower lobes (arrow on sagittal reconstruction).
Two days later a sputum test was positive for COVID-19.
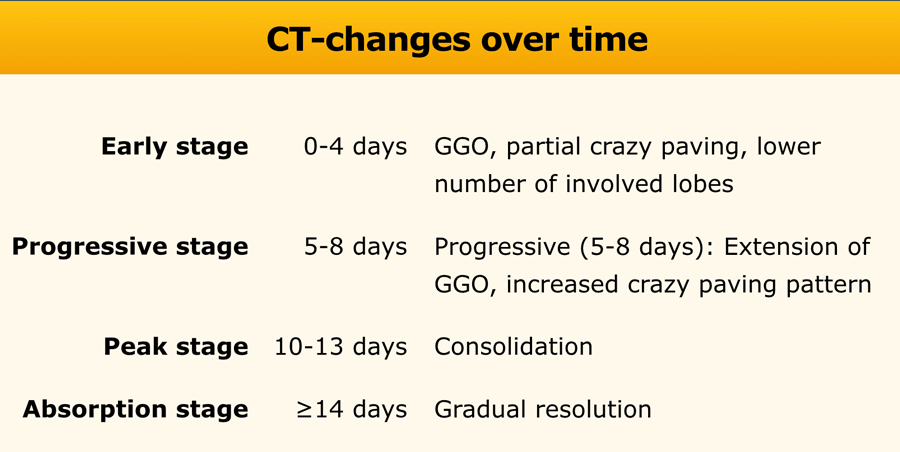
Changes over time
Advanced-phase disease is associated with a significantly increased frequency of:
- GGO plus a reticular pattern (crazy pavin)
- Vacuolar sign
- Fibrotic streaks
- Air bronchogram
- Bronchus distortion
- Subpleural line or a subpleural transparent line
- Pleural effusion
This 59 year old female had a history of ten days of fever and five days of coughing.
The O2 saturation was 89 and her respiratory rate was 30/min (normal: 12-18).
There are widespread GGO's without consolidation. No architectural distortion.
This was reported as early phase COVID-19.
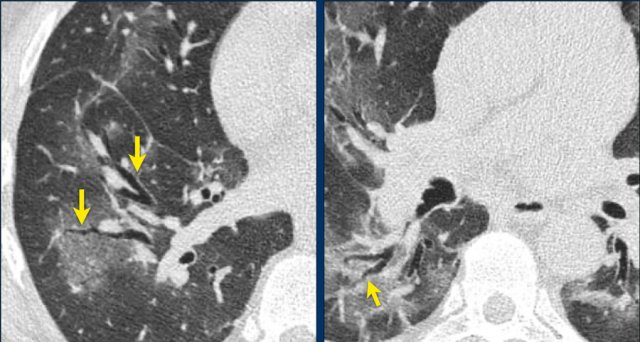
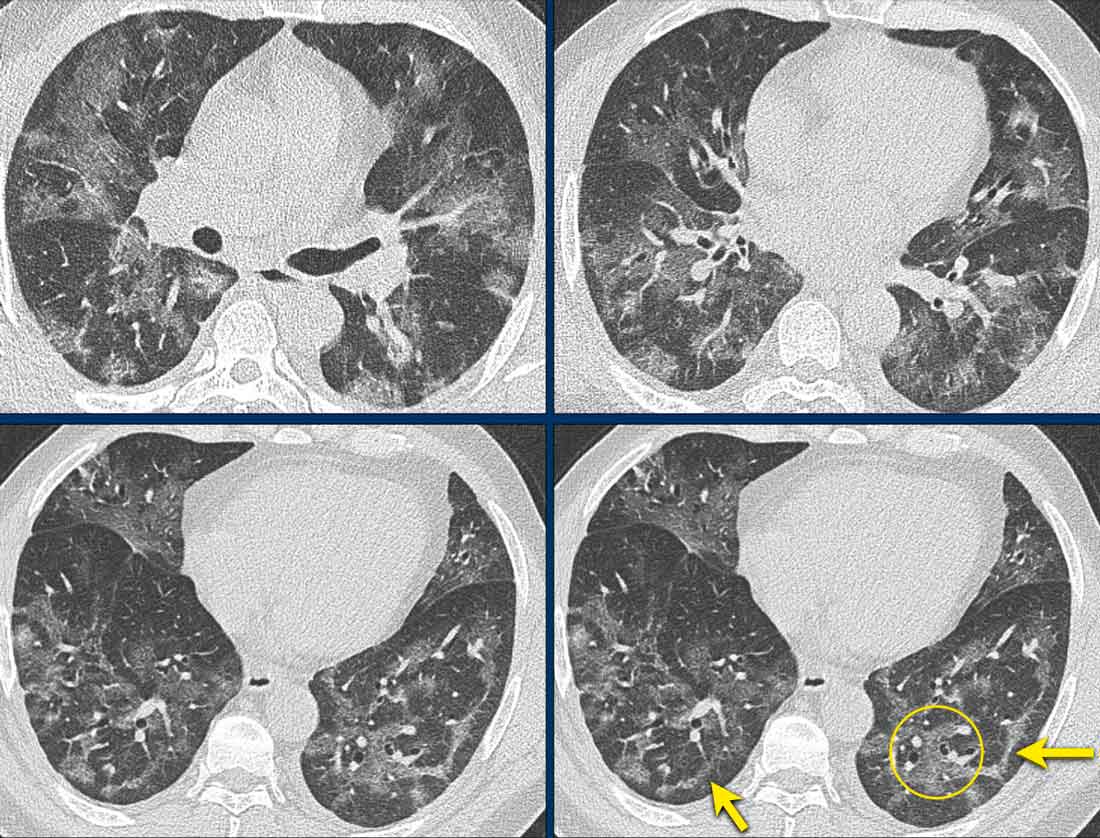
These images are of a 49 year old male with fever, cough and a low saturation.
The images show:
- Bilateral areas of GGO.
The ground glass density is more pronounced - Fibrotic bands (arrows).
- Dilated vessels in affected area (circle).
Based on the CT-findings COVID-19 infection was assumed to be highly likely - late phase.
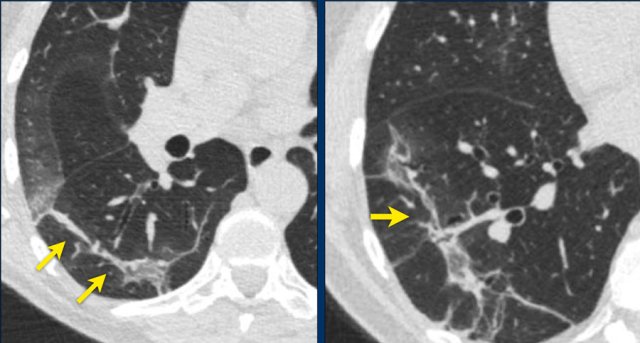
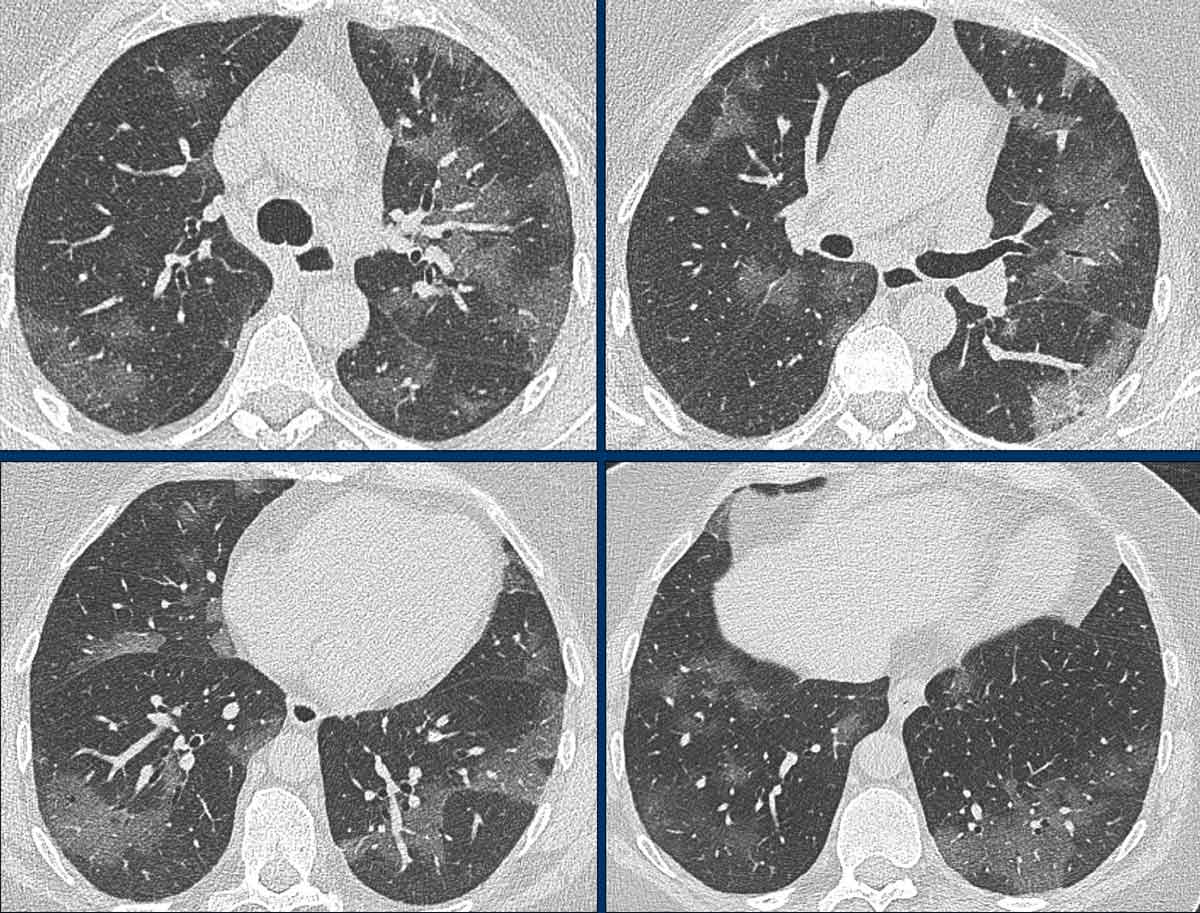
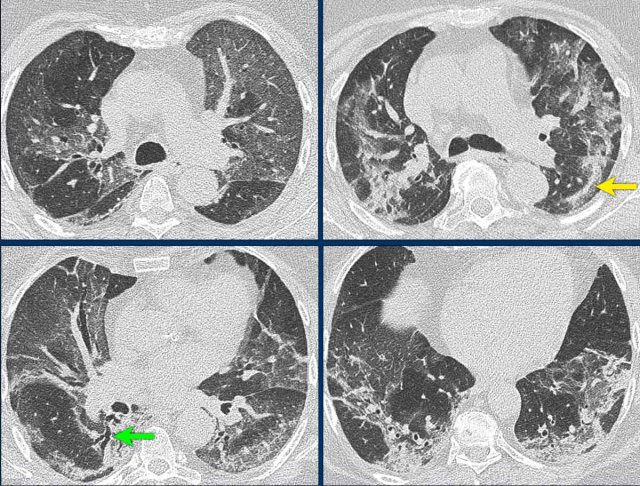
This patient had fever for one week with some abdominal pain and diarrhoea.
On the day of admission she had a dry cough and complained of dizziness.
The O2-saturation was low.
The PCR-test was not known and a CT was performed for triage.
The images show:
- Bilateral subpleural GGO's
- Consolidation in right lower lobe with traction bronchiectasis (green arrow).
- Fibrous bands (yellow arrow).
Based on the CT-findings COVID-19 infection was assumed to be highly likely - late phase.
CT Report
In the tabel a checklist of CT findings to mention in the report.
In the first four days after the presentation of the complaints, the CT is not sensitive as initial test as 50% of patients may have a normal CT.
After these first four days, the CT has a very high sensitivity.
Chest radiograph
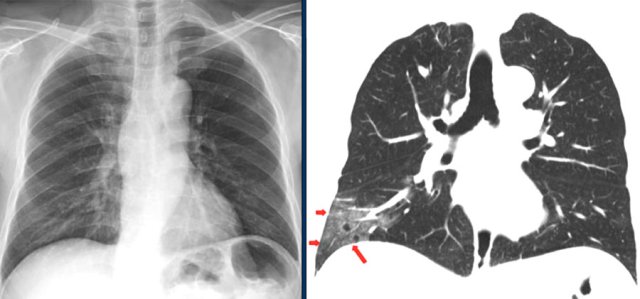
The chest film is insensitive early in the disease.
Here a comparison of a chest radiograph and CT image.
The ground glass opacities in the right lower lobe on the CT (red arrows) are not visible on the chest radiograph, which was taken 1 hour prior to the CT-study (1).
Chest-films can be useful in the follow-up of the disease.
These x-rays are of a patient with COVID-19.
On admission to the hospital the chest film was normal.
Four days later the patient is on mechanical ventilation and there are bilateral consolidations on the chest film.
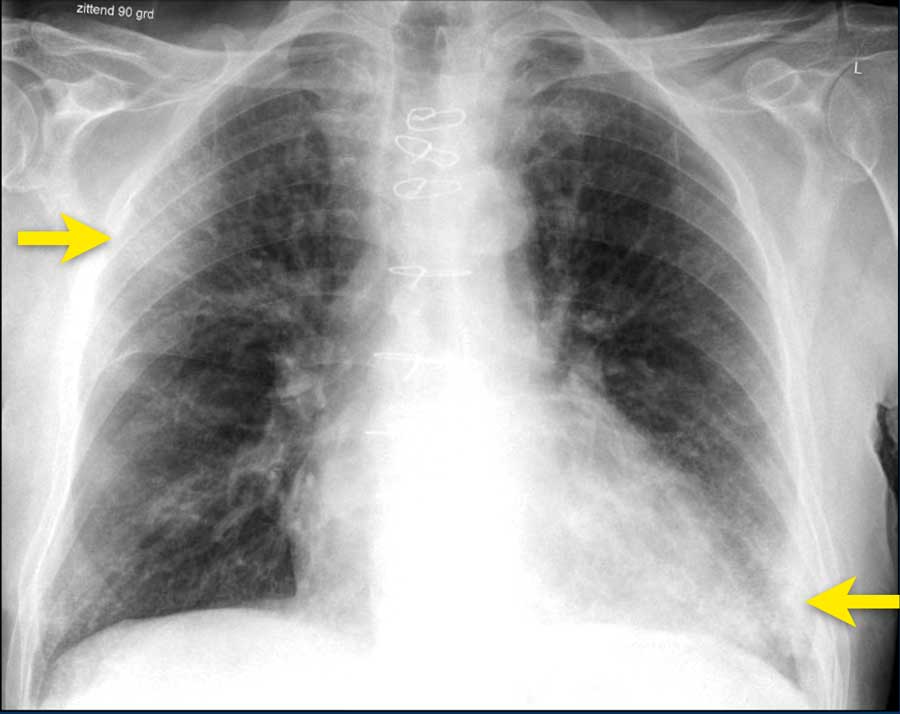
Chest film of a 83 year old male with mitral insufficiency, pulmonary hypertension and atrial fibrillation with COVID-19 infection.
Ground-glass opacification and consolidation in right upper lobe and left lower lobe (arrows).
A series of chest films of a 72-year-old woman admitted with acute respiratory failure, fever (38ºC) and dyspnoea.
She was tachypneic (30bpm), with lymphopenia and low oxygen saturation (SpO2 85%).
Patient presented to the emergency department two days earlier with fever (up to 38.6ºC), dry cough, odynophagia and general malaise.
She was discharged from hospital because she did not present alarm criteria at that time.
The patient required mechanical ventilation and was admitted to intensive care.
During her stay in ICU, poor evolution to respiratory distress syndrome and to multi-organic failure.
The patient died 24 hours later.
Imaging findings:
- At admission: Ill-defined bilateral alveolar consolidation with peripheral distribution.
- 4 hours later: Radiological worsening, with affectation of lower lobes. Endotracheal tube and central venous line were required.
- 24 hours: Bilateral alveolar consolidation.
- 48 hours: Radiological worsening. Bilateral alveolar consolidation with panlobar affectation.
- 72 hours: Bilateral alveolar consolidation with panlobar affectation, with typical radiological findings of ARDS. 24 hours later the patient passed away.
Possible role of CT
CT can play a role in:
- Triage of patients:
- no COVID-19
- possible or most likely COVID-19
- severity of the disease - Prediction of worsening
- Prediction of improvement
- Problem solver
Triage
Some published clinical guidelines recommend chest CT for patients with suspected COVID-19.
The decision to use of CT for triage depends on many considerations:
- a priori chance of COVID-19 infection.
- CT availability, for instance can one CT be used as Corona-CT or is there a CT near the emergency room.
- clinical suspicion in patients with negative PCR.
Video cases of CT Chest
...
This is a 67 year old woman who was coughing for one week and now presented with shortness of breath.
This is a CT-scan of a 53 year old woman at admission.
There are 2 areas with a halo sign, some areas of ground-glass and consolidations in the lower lobes.
Based on the CT-findings she was suspected of having COVID-19.
The PCR-test the next day was positive.
60 year old male with complaints of fatigue and coughing for one week.
COVID-19 Lung Disease: a pulmonary vasculopathy
Watch the presentation by Dr Graham Lloyd-Jones, Director of Radiology Masterclass, given on November 11th 2020 at the annual (virtual) conference of the British Society for Haematology, titled - What can the Radiology tell us about the vasculopathy of COVID-19 lung disease?