Coronary Artery Disease-Reporting and Data System 2.0
Examples for the different Cad-Rads categories
Csilla Celeng, Richard Takx, Robin Smithuis and Tim Leiner
University Medical Center Utrecht, Amsterdam University Medical Center, Mayo Clinic, Rochester, USA and Alrijne hospital Leiden
Publicationdate
CAD-RADS is the Coronary Artery Disease-Reporting
and Data System.
CAD-RADS is developed to standardize reporting of coronary CTA, to improve communication and to guide therapy.
The original article was published in 2016 by the
Society of Cardiovascular Computed Tomography (SCCT), the American College of
Radiology (ACR) and the North American Society for Cardiovascular Imaging
(NASCI) and it has been endorsed by the American College of Cardiology (ACC) (1).
CAD
RADS 2.0
In
2022 CAD RADS was updated to version 2.0 (2).
Similar to the
original CAD-RADS version, stenosis severity determines the CAD-RADS score
(from 0 to 5).
New in the current version is the incorporation of plaque burden
(from P1 to P4) and an update of the modifiers.
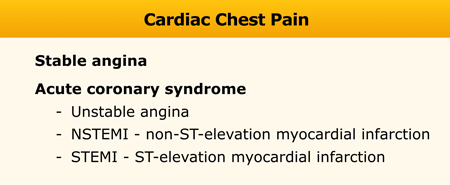
Understanding Chest pain
Cardiac chest pain can be categorized into stable angina, unstable angina, non-ST-elevation myocardial infarction (NSTEMI) and ST-elevation myocardial infarction (STEMI) (2,3).
The latter three are called acute coronary syndromes.
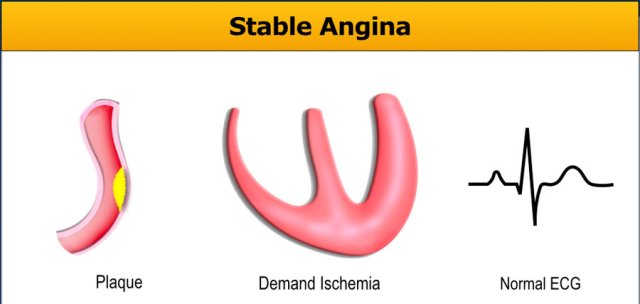
Stable angina
Stable angina is characterized by exertional chest pain induced by exercise, stress or emotion.
It is a mismatch between myocardial oxygen demand and supply due to the presence of atherosclerosis, microvascular dysfunction or spasm.
This type of angina is relieved by rest or administration of nitroglycerin.
Troponin-levels are normal.
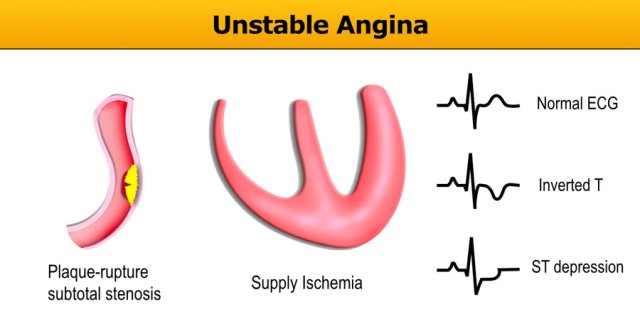
Unstable angina
Unstable angina pectoris (UAP) is defined as chest pain which occurs at rest or minimal exertion and is characterized by the absence of cardiomyocyte necrosis and normal troponin-levels (3).
UAP is caused by plaque rupture with thrombus formation causing partial occlusion of the affected vessel.
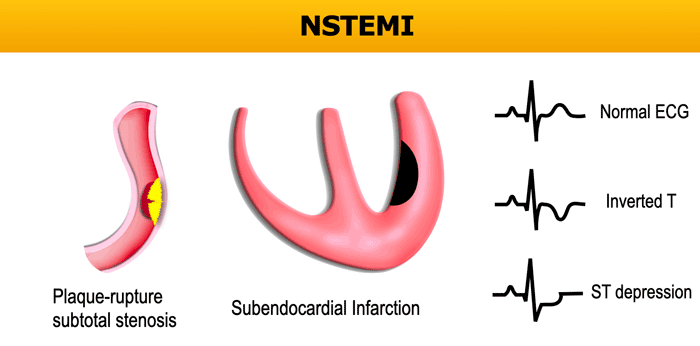
NSTEMI
NSTEMI or non-ST-elevation myocardial infarction is the result of plaque rupture and thrombus formation which causes partial occlusion and subendocardial infarction with elevated troponin-levels.
The ECG can be normal, or abnormal with inverted-T or ST-depression.
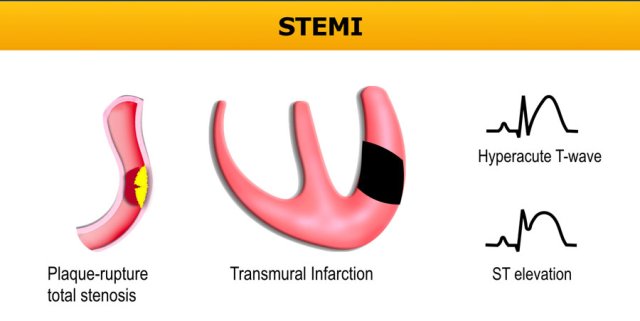
STEMI
STEMI or ST-elevation myocardial infarction is characterized by complete occlusion of the lumen leading to a transmural infarction with elevated troponin-levels.
The ECG is abnormal with ST-elevation or a hyperacute T-wave.
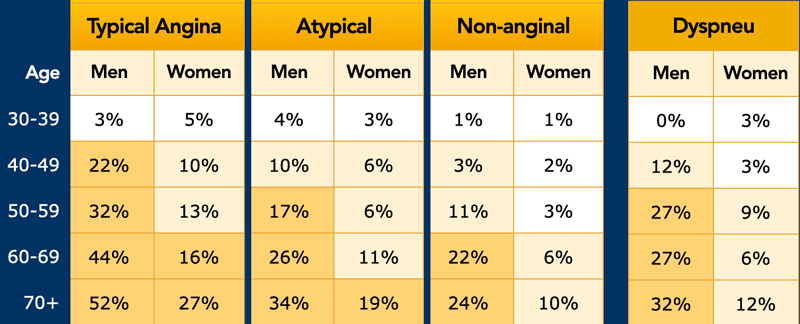
Target population for coronary CTA
According to the guidelines of the European Society of Cardiology non-invasive imaging (including CTA) can be used in all patients with a pre-test probability of >15% and can be considered in those with a pre-test probability between 5-15% (4).
The pre-test probability is based on the age and gender of the patient combined with the type of complaints: typical angina, atypical angina or non-anginal chest pain (Table).
Typical angina is:
- substernal chest discomfort of characteristic quality and duration
- provoked by exertion or emotional stress
- relieved by nitrates or rest within minutes.
Atypical angina meets two of the before mentioned criteria.
Non-anginal chest pain lacks these criteria or meets only one.
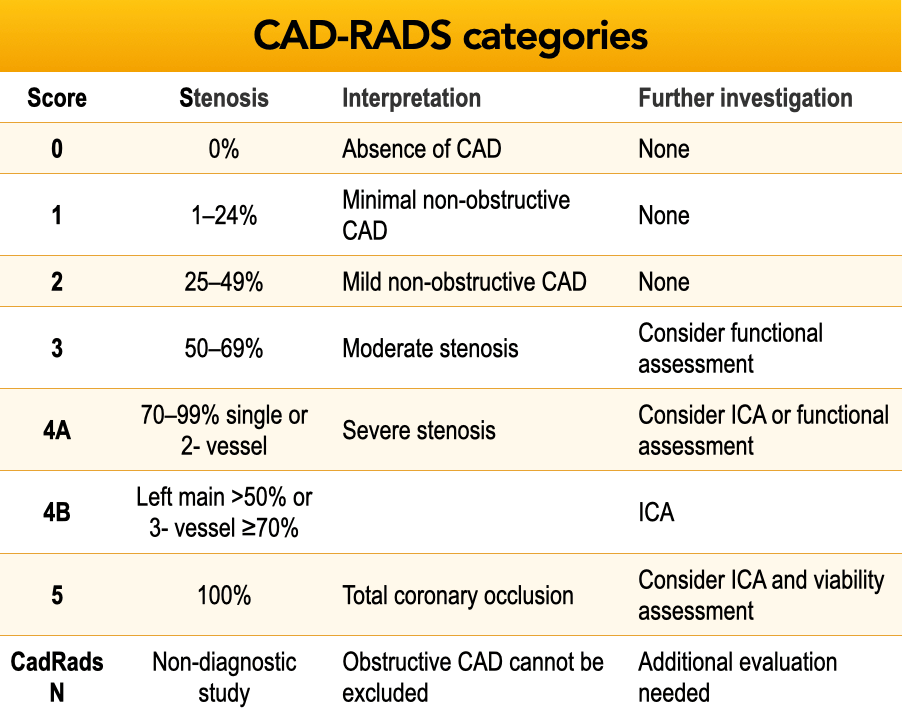
CAD-RADS
Assessment of stenosis degree
Cad-Rads categories of the different coronary segments are based on the SCCT stenosis grading and coronary segmentation diagram (5).
All coronary arteries >1.5 mm diameter are graded for stenosis severity and the clinically most relevant stenosis has to be documented.
Cad-Rads 1 category also includes the presence of plaque with positive remodeling but no stenosis.
Cad-Rads 4 category is divided into two subcategories:
- 4A = single or two-vessels disease with severe (70-99%) stenosis
- 4B = in the left main >50% stenosis or three-vessel disease with >70% stenosis.
In patients with CAD-RADS 4A the next step can be ICA or functional assessment, i.e. CT-FFR, CTP, stress testing (exercise tolerance test, stress echocardiogram, SPECT, PET or cardiac MRI).
In patients with Cad-Rads 4B ICA is recommended.
Click here to go to case 1 for an example of quantitative assessment of stenosis degree.
The same assessment in this table.
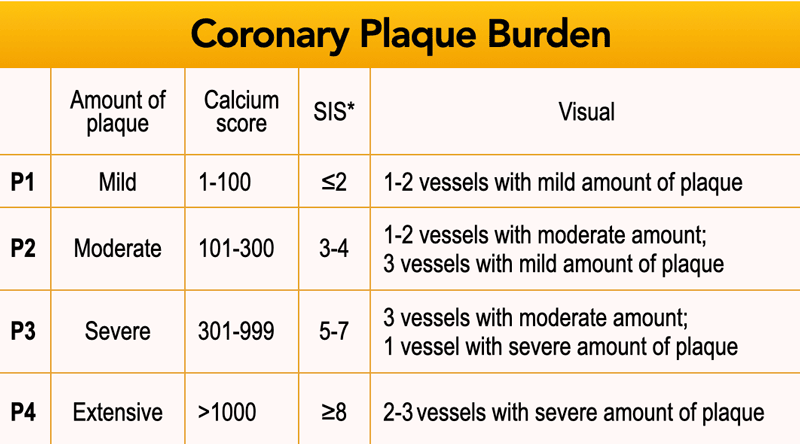 *SIS - Segment involvement score. SIS is a semiquantitative measure derived from the coronary CTA scan (7). For each of the 16 coronary segments a score of 1 is added if any plaque is present for a maximum of 16, or 17 in case a ramus intermedius is present.
*SIS - Segment involvement score. SIS is a semiquantitative measure derived from the coronary CTA scan (7). For each of the 16 coronary segments a score of 1 is added if any plaque is present for a maximum of 16, or 17 in case a ramus intermedius is present.
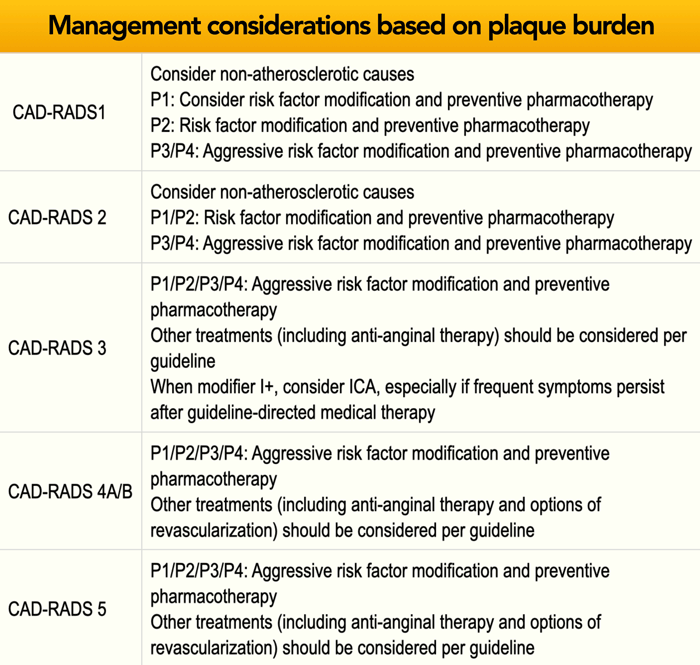
P - Overall plaque burden sub-classification
In CAD-RADS 2.0 overall plaque
burden has been added ranging from P1 (mild) to P4 (extensive).
Plaque burden
should be listed after highest stenosis degree with addition of symbol /
(slash) (e.g. CAD-RADS 3/P2).
Plaque burden should be determined
by the technique which is considered most appropriate at the local institution.
This includes calcium score or segment involvement score (SIS) or based on
visual assessment.
Note that CAD-RADS 0 denotes absence of stenosis or plaque,
therefore P0 is not needed as a classification.
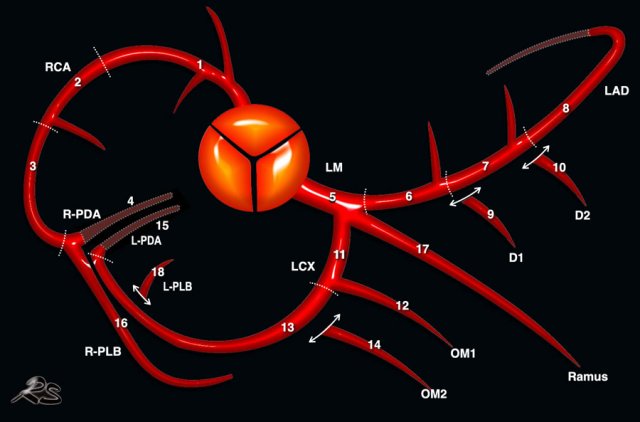 Society of Cardiovascular Computed Tomography (SCCT) coronary segmentation diagram (15). Click to enlarge.
Society of Cardiovascular Computed Tomography (SCCT) coronary segmentation diagram (15). Click to enlarge.
This coronary segment diagram of the Society of Cardiovascular Computed Tomography is used to indicate where the stenoses are located (6).
LM: left main
LAD: left anterior descending artery
D1: diagonal 1
D2: diagonal 2
LCX: circumflex artery
OM1: obtuse marginal 1
OM2: obtuse marginal 2
L-PDA: PDA from LCX
PLB: posterolateral branch; L-PLB: PLB from LCX.
RCA: right
coronary artery
PDA: posterior descending artery
R-PDA: PDA from RCA
PLB: posterolateral branch; R-PLB: PLB from RCA.
Dashed lines represent the division between LM, LAD and LCX as well as the proximal, mid and distal segments of LAD, LCX and RCA.
Cad-Rads Modifiers
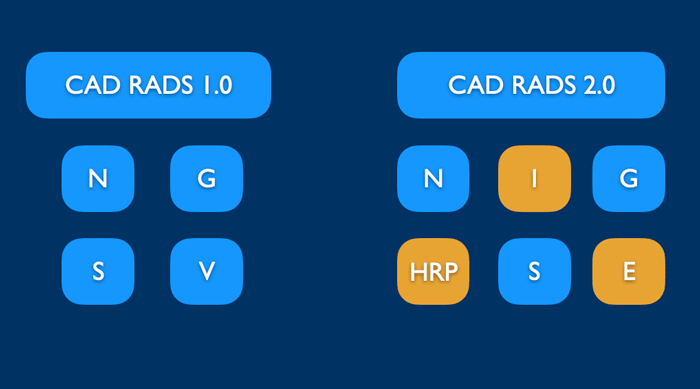
In CAD RADS 1.0 there were four modifiers.
In CAD RADS 2.0 there are 6 modifiers that can be added to the Cad-Rads category:
- N: indicates that a study is non-diagnostic
- HRP: high-risk plaque (replaces V-vulnerable plaque)
- I: ischemia
- S: presence of stents
- G: coronary artery bypass grafts
- E: exceptions
A modifier is named after the highest stenosis degree with the use of symbol / (slash).
For instance Cad-Rads 3/S.
 Example of a non-diagnostic scan. Both the RCA and LCX are blurred due to motion artifacts, resulting in CAD RADS N.
Example of a non-diagnostic scan. Both the RCA and LCX are blurred due to motion artifacts, resulting in CAD RADS N.
Modifier N - nondiagnostic
If not all segments (>1.5 mm diameter) are diagnostic (e.g. motion artifacts), modifier N should be listed.
There are two ways of listing modifier N:
- In case of a non-diagnostic segment and the presence of no (0%), minimal (< 25%) or mild (25-49%) stenosis category CAD-RADS N should be used (no stenosis grade should be listed, since coronary CTA is not able to guide patient management).
- In case of stenosis degree ≥ 50% in one diagnostic segment the patient should be categorized as CAD-RADS 3/N.
Overall plaque burden
should also be reported for non-diagnostic scans (N), if total coronary plaque
burden can be assessed reliably.
In case of stenosis degree < 50% N should be
placed before category P (e.g. CAD RADS N/P2).
If stenosis ≥ 50% then P should precede N (e.g. CAD RADS
3/P2/N).
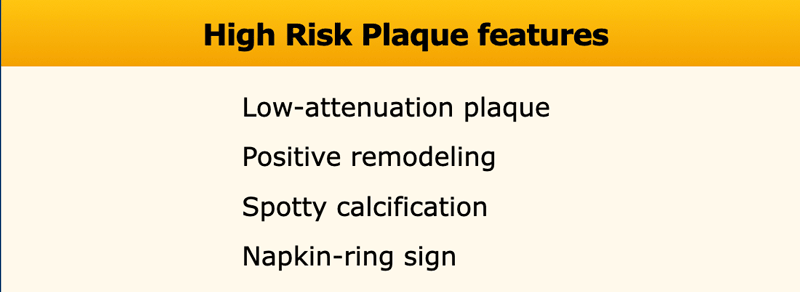
Modifier HRP - high-risk plaque
The term “vulnerable plaque” has been replaced by “high-risk plaque
features” as modifier “HRP”.
High-risk plaque features include: low-attenuation plaque, positive remodeling,
spotty calcification and napkin-ring sign. If two or more of these
features are present modifier “HRP” should be added to the CAD-RADS category.
There are three plaque types on coronary CTA:
- calcified
- partially calcified
- non-calcified
Calcified plaque is an atherosclerotic plaque in which the entire plaque appears as
calcium density (>130 HU on non-enhanced CT).
The previous terminology “hard plaque” is not recommended.
Partially calcified plaque is an atherosclerotic lesion with 2
components of which one is calcification.
The previous term was “mixed plaque”, which is no longer recommended.
Non-calcified plaque is a plaque without calcium content. The use of “soft-plaque”, “low-density plaque” and “fibrous plaque” should be avoided (8).
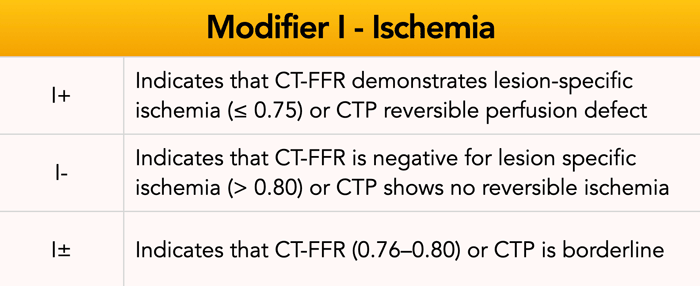
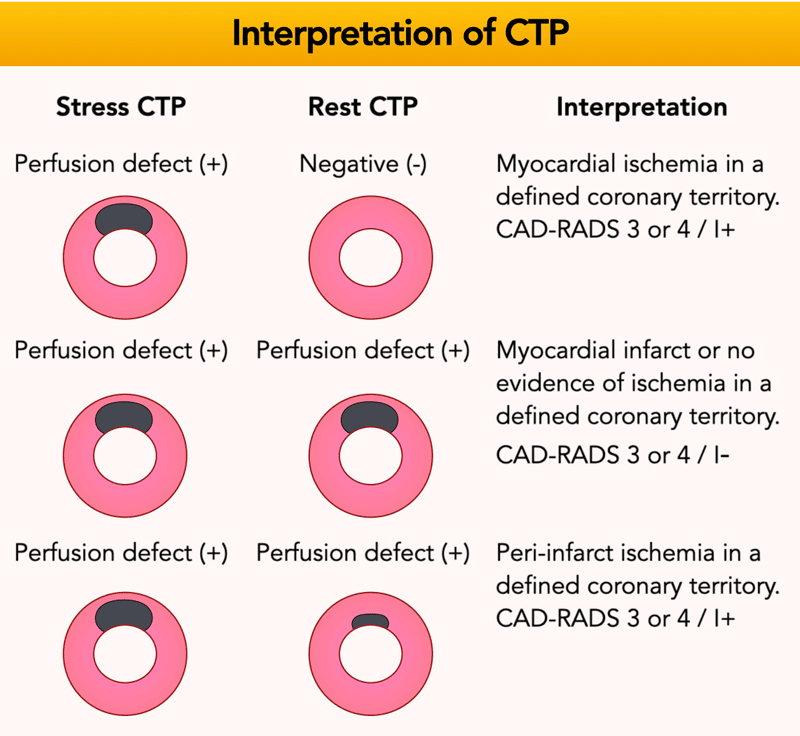
Modifier I - ischemia
CT-FFR (computed tomography fractional flow reserve) and stress CTP (computed tomography perfusion) are CTA derived non-invasive imaging techniques which allow to better define the hemodynamic significance of a stenosis ranging from 50 to 90% (CAD-RADS 3 and 4A).
CAD-RADS 2 lesions can be also considered if there is a proximal stenosis ≥ 40%, including the presence of high-risk plaque features.
FFR-CT is a digital 3D model of simulated blood flow in the coronary arteries.
This figure shows a hemodynamically significant
stenosis in the LAD (0.58) and distal RCA (0.75).
This means the presence of
ischemia; modifier I + should be used.
In case of a mismatch between CT-FFR or CTP and CCTA results, an ischemic segment without a concordant anatomic lesion, should be classified as I- if the reader is confident that this is a false-positive result by CT-FFR or CTP or I± if it is indeterminate and there is questionable and discrepant interpretation.
Please note that patients with
prior myocardial infarction and fixed perfusion defects without myocardial
ischemia on CTP should
be classified as I-.
The presence of myocardial infarction should be documented
in the report.
Modifier S - stent
The presence of a stent is indicated by modifier “S”.
Examples
- If a patient has a stent, showing no in-stent restenosis and a mild (25-49%) stenosis in the coronaries, this patient classifies as CAD-RADS 2/S.
- Similarly, a patient with no in-stent restenosis but severe (70-99%) stenosis in a coronary other than LM classifies as CAD-RADS 4A/S.
- If there is a severe (70-99%) in-stent restenosis in a coronary other than LM, this patient classifies as CAD-RADS 4A/S.
- If the stent is non-diagnostic and there is no >49% stenosis present in the coronaries, the patient classifies as CAD-RADS N/S.
Note: the location of the stenosis does not matter, when using
CAD-RADS.
What matters is that the patient has a severe stenosis and needs further
management.
Please note: total coronary plaque burden should also be added and is placed before the modifier S.
 A. example of LIMA-LAD without stenosis. B.example of SVG to posterior descending artery also with no stenosis in the graft. NB: there is a severe stenosis distal to the SVG, which is the bypassed stenosis and as of that is not considered for CAD-RADS classification.
A. example of LIMA-LAD without stenosis. B.example of SVG to posterior descending artery also with no stenosis in the graft. NB: there is a severe stenosis distal to the SVG, which is the bypassed stenosis and as of that is not considered for CAD-RADS classification.
Modifier G - graft
The presence of coronary artery bypass grafts is indicated by modifier
“G”.
Importantly, a bypassed stenosis is not considered for CAD-RADS stenosis classification.
Examples:
- If a patient has a patent LIMA-LAD graft (left internal mammary artery graft to left anterior descending artery) with no stenosis in the graft but there is a mild (25-49%) stenosis in the coronaries- in addition to the “expected” LAD bypassed stenosis – this patient classifies as CAD-RADS 2/G.
- If a patient has an occluded LIMA-LAD graft, a patent SVG (saphenous vein graft) to the RCA and a severe (70-99%) stenosis in the coronaries, this patient would classify as CAD-RADS 5/G (the highest stenosis is graded).
Note: the location of the stenosis does not matter, when using CAD-RADS.
What matters is that the patient has an occlusion and needs further management.
Please note: Total coronary plaque burden (combined assessment of native coronary arteries and bypass grafts) should also be added and is placed before the modifier G.
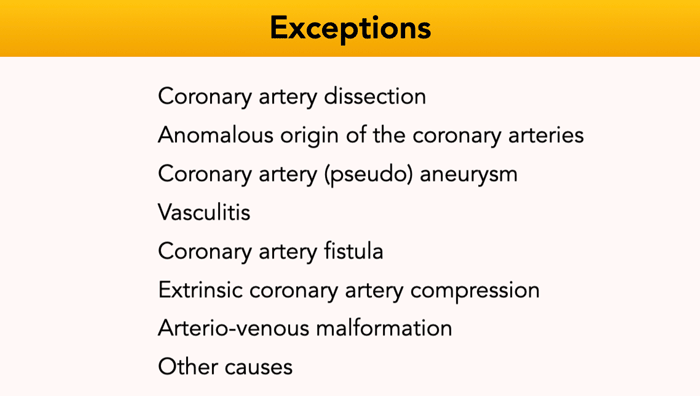
Modifier E - exceptions
Modifier E is exceptions and non-atherosclerotic abnormalities.
The presence of non-atherosclerotic
abnormalities should be added as modifier “E” to CAD-RADS score.
Non-atherosclerotic luminal narrowing of the coronary arteries may require
disease-specific management or subspecialty referral.
This image is of a patient with Kawasaki disease.
There is a coronary artery aneurysms (8 mm and 6 mm diameter)
of the LAD.
Please also note the presence of partially calcified plaque in the proximal aneurysm.
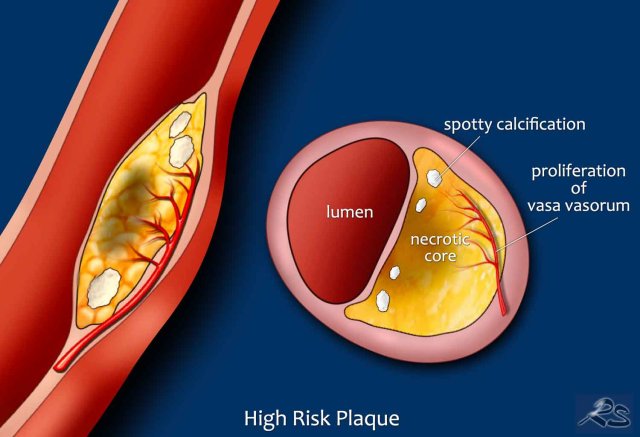
CTA features of stable and high risk plaque
The morphology of high-risk plaques, which are thought to underly acute coronary syndrome, differs from stable plaques.
Stable plaques
On histology, stable plaques are characterized by large calcifications,
fibrotic tissue and smaller lipid pools.
High-risk plaques
Conversely, unstable plaques can contain spotty calcifications, large-lipid
pool (necrotic core), which is covered by a thin fibrous cap. These
plaques are sometimes referred to as thin-cap fibroatheroma (TCFA).
Some of
these high-risk plaque features can be identified by CTA.
Low-attenuation plaque
Lesions associated with plaque rupture frequently have a large lipid rich core.
Lipid on CT appears as low attenuation.
Plaques with < 30 HU on CTA were found to be present significantly more often in patients with acute coronary syndrome (9).
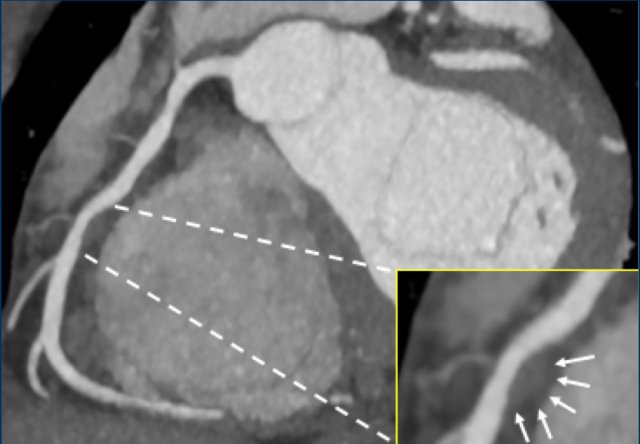
Positive remodeling
Positive remodeling is defined as a compensatory outward enlargement of the vessel wall at the site of the atherosclerotic lesion with preservation of the coronary lumen (8).
On histology plaques with positive remodeling show a higher lipid content and abundance of macrophages (9).
Patients with positive remodeled plaques can present with an acute coronary syndrome without any prior cardiac history.
An example of positive remodeling of a non-calcified plaque in the mid RCA.
There is outward growth of the plaque with minimal stenosis of the lumen.
Another example of positive remodeling of a calcified plaque in the proximal LAD.
Again, the plaque is outward from the lumen causing no stenosis in the LAD.
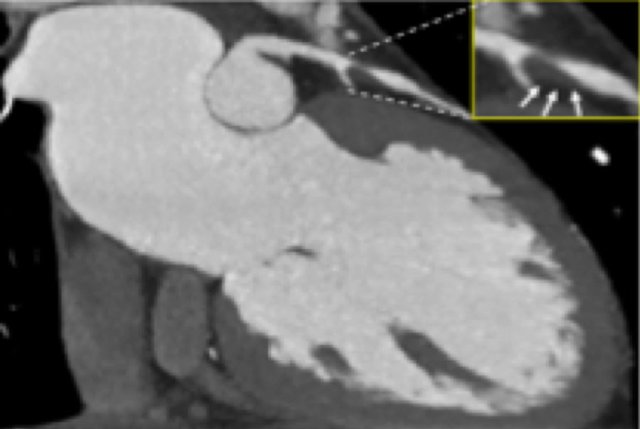
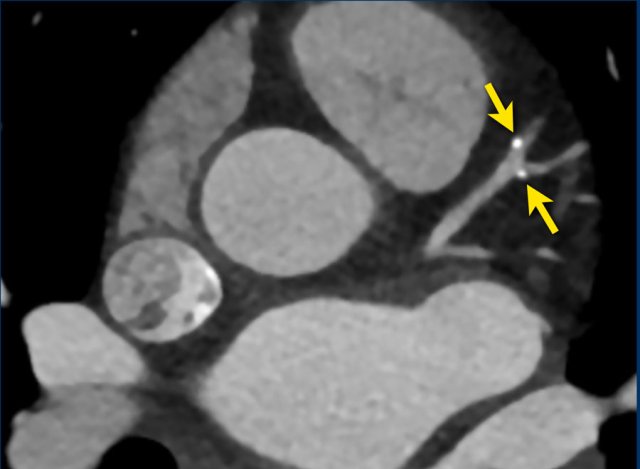
Spotty calcification
Spotty calcifications are usually defined as calcifications < 3
mm.
Small spotty calcifications on CTA are associated with high-risk plaques (12).
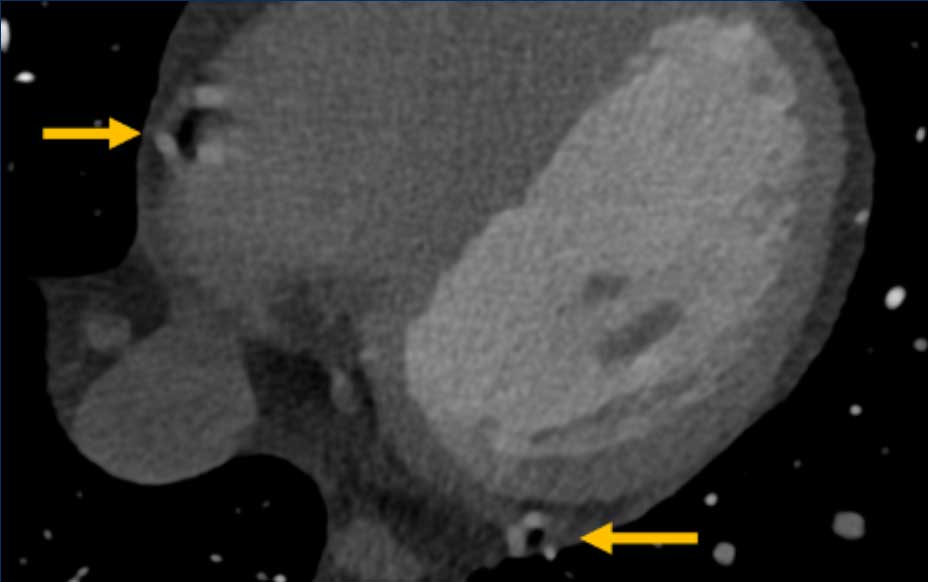
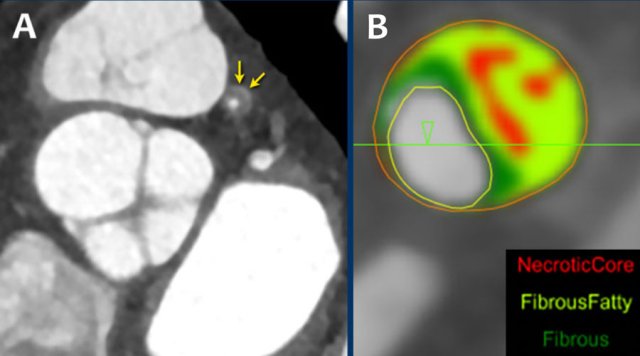 A: On the coronal image the so-called napkin-ring sign (dark area adjacent to the lumen, surrounded by a higher “ring-like” attenuation (white arrows). B: Tissue characterization on CT by HU number
A: On the coronal image the so-called napkin-ring sign (dark area adjacent to the lumen, surrounded by a higher “ring-like” attenuation (white arrows). B: Tissue characterization on CT by HU number
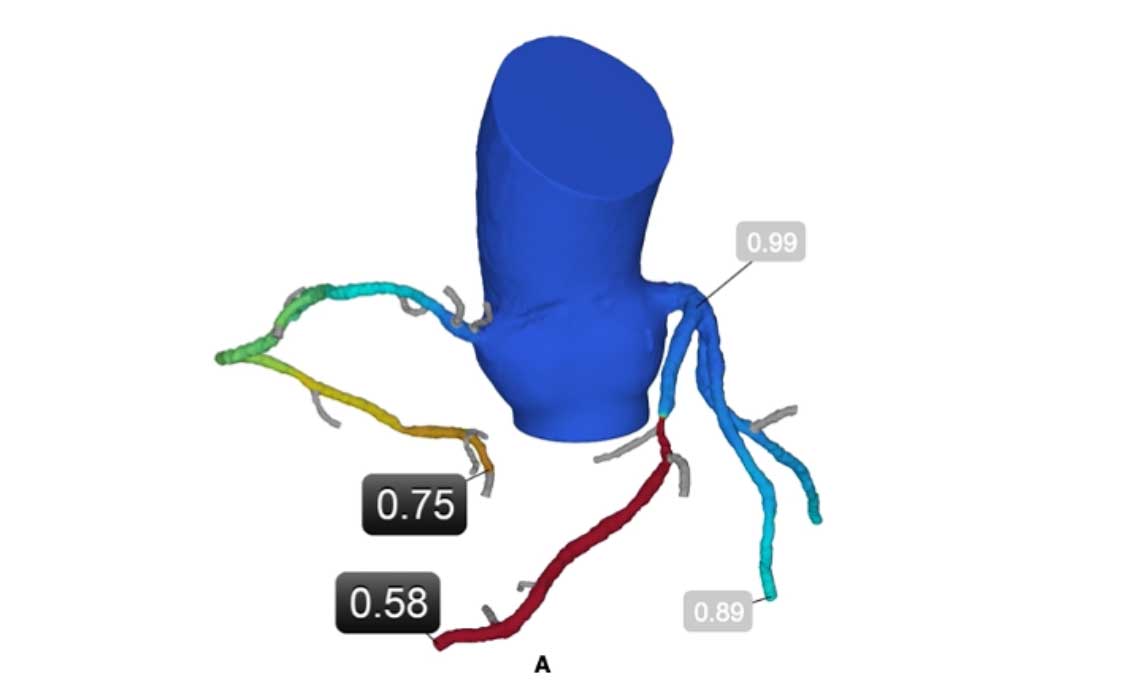
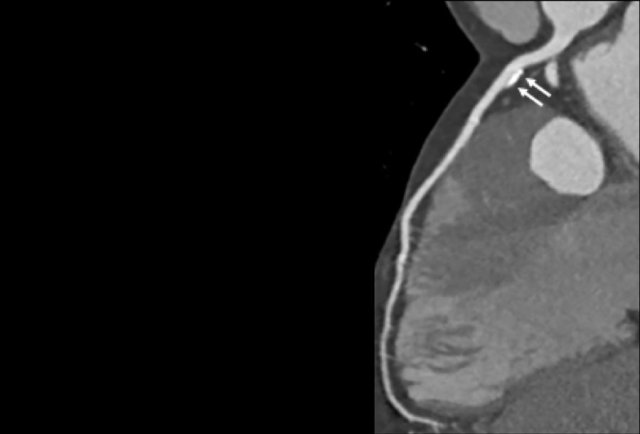
Napkin-ring sign
The Napkin-ring sign is a qualitative high-risk plaque feature
on CTA (13).
It is defined as a central low-attenuation area adjacent to the coronary lumen
and a higher “ring-like” attenuation tissue surrounding this central area (14).
On histology, the area of low-attenuation corresponds to the necrotic core,
while the “ring-like” outer area correlates with fibrous plaque tissue.
The Napkin-ring sign is strongly associated with major adverse
cardiovascular events (15).
Coronary CTA protocol
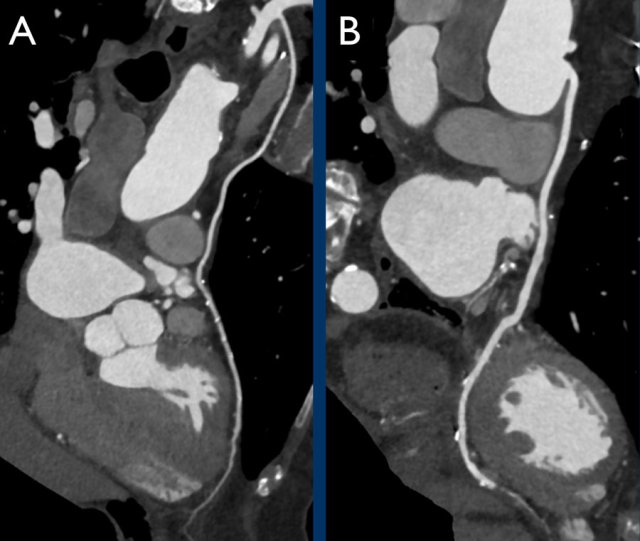
 Example of a CTA scan performed on the same scanner in the same patient without (A) and with (B) administration of nitroglycerin, showing the increased diameter of the LAD. Due to the vasodilatory effect nitroglycerine increases the number of assessable (>1.5 mm diameter) segments.
Example of a CTA scan performed on the same scanner in the same patient without (A) and with (B) administration of nitroglycerin, showing the increased diameter of the LAD. Due to the vasodilatory effect nitroglycerine increases the number of assessable (>1.5 mm diameter) segments.
Coronary CTA basics are:
- Administration of betablockers - if the heart rate > 65 BPM.
- Administration of nitroglycerine.
- Prospective ECG-gating or retrospectively gated helical mode.
- Calcium score reported in the form of Agatston score.
- Post-processing: axial image review, multiplanar reformation and maximum intensity projection.
- Optional image review: curved multiplanar reformation and volume rendered reconstruction.
Extra cardiac findings
Of patients presenting with acute chest pain 5-10% suffer from STEMI,
15-20% from NSTEMI, 10% from UAP, 15% from other cardiac conditions and in the
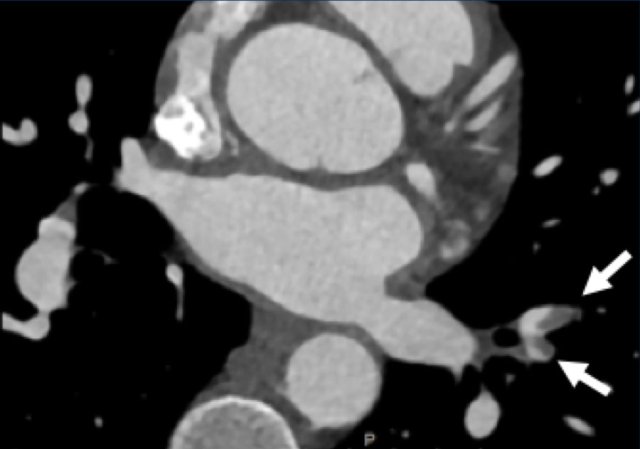
remaining approximately 50% non-cardiac diseases are the underlying cause (4).
Non-cardiac conditions include acute aortic syndrome (e.g. intramural hematoma,
penetrating atherosclerotic ulcer, dissection or rupture), pulmonary embolism
(see arrows in figure), pericarditis, or other intra-thoracic pathologies.
For these conditions the use of double or triple-rule-out CTA could provide an
alternative explanation for the symptoms.
Image
Multiple pulmonary emboli (arrows).
Examples
case 1 - CAD-RADS 2/P1
First, scroll through the scan.
Not all images are included. Some images without any abnormalities are skipped
from the series.
How would you describe the findings on the coronary CTA?
The findings are:
- Agatston score of this patient was 14 (P1). Please, also note the calcification of the aortic valve.
- Some partially calcified and calcified plaques are present in the LAD with mild stenosis (25-49%).
- Calcified-plaque in the LCX causing minimal stenosis (<25%).
- Non-calcified plaque in the distal RCA causing minimal stenosis (<25%).
- This patient classifies
as CAD-RADS 2/P1, which means no further workup is needed.
case 2 - CAD-RADS 5/P2/S
First, scroll through the CTA images.
How would you describe the findings on the coronary CTA?
The findings are:
- Stent in the mid LAD with low-attenuation within the stent suggestive of minimal in-stent restenosis (<25%). Non-calcified plaque distal to the stent causing mild stenosis (25-49%). Notice bridging on a short segment in the distal LAD.
- Non-calcified plaque in the LCX causing mild stenosis (25-49%).
- Occlusion of the proximal OM1 branch with distal filling.
- Calcified and non-calcified plaques in the proximal RCA causing mild (25-49%) stenosis.
- Total plaque burden is moderate based on SIS (four segments including proximal RCA, mid LAD, prox LCX and OM1).
Due to the occlusion of OM1 branch and presence of the stent, this case
reads as CAD-RADS 5/P2/S, which means that this patient needs further
diagnostic workup.
case 3 - Calcium score 0 and severe stenoses.
First, scroll through the CTA images.
How would you describe the findings on the coronary CTA?
The findings are:
- The total calcium score of 0 indicates the absence of calcified plaque in the coronary tree.
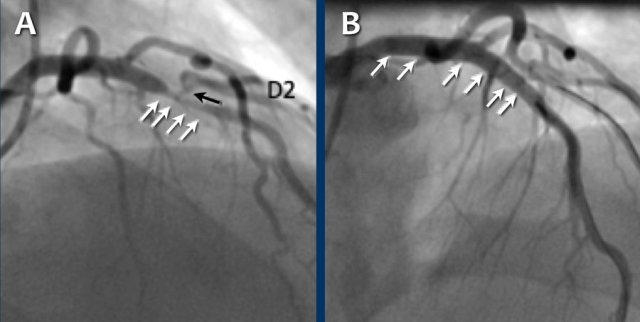
- Severe stenosis (70-99%) in the mid LAD and D2 branch.
Continue with the next images of the same patient...
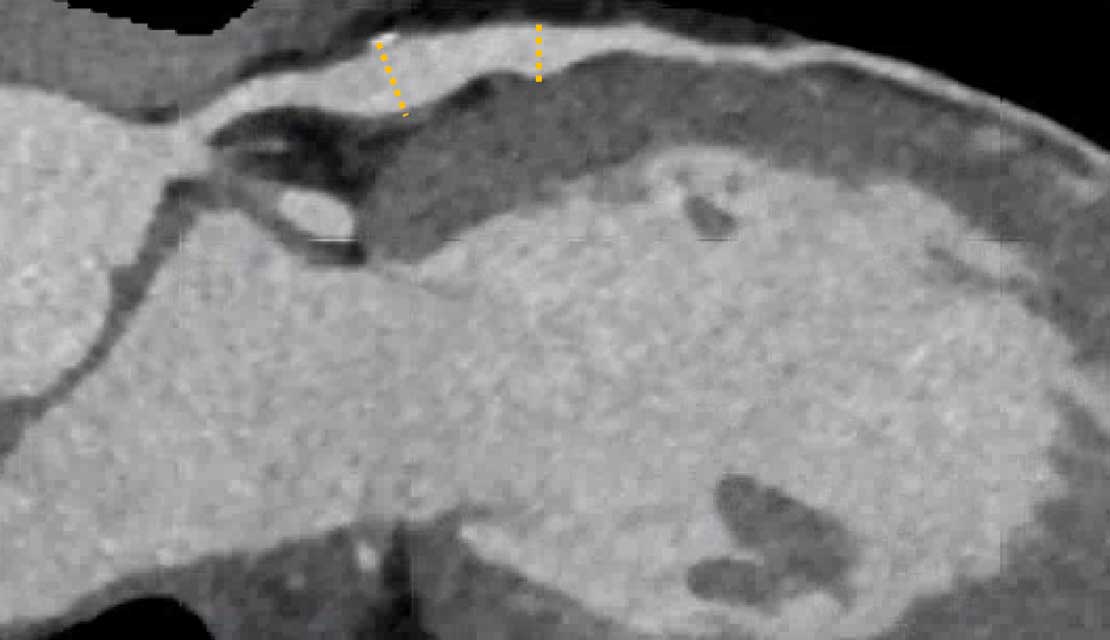
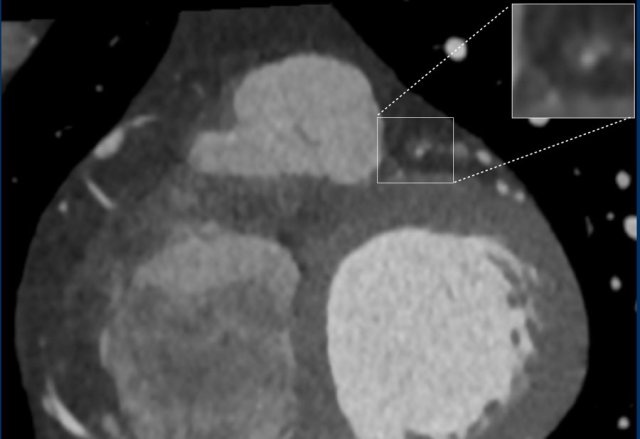
Same patient. First, study the CTA image.
How would you describe the findings?
The coronal image shows a central low-attenuation area around the lumen
of the LAD.
This low-attenuation area is surrounded by a higher attenuation
area.
This finding is the earlier discussed napkin-ring sign, which is a high-risk
plaque feature.
This patient classifies as CAD-RADS 4A/P1/HRP.
Continue with the next images of the same patient...
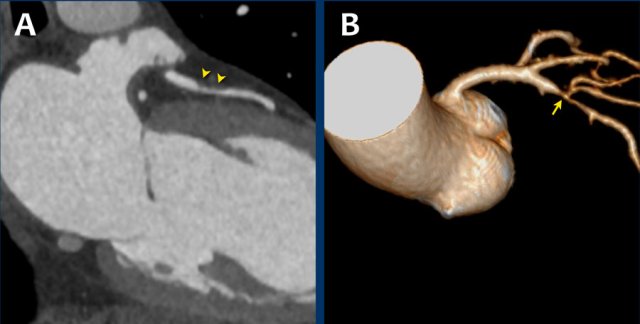
Same patient.
Double-oblique (A) and volume-rendered (B) images of the LAD showing the
location and the length of the plaque.
Also, the stenosis in the D2 branch of the LAD can be appreciated on the volume
rendered reconstruction.
Due to the degree of stenosis and the presence of napkin-ring sign (visible on
axial images) this patient underwent ICA where the presence of severe stenosis
was confirmed.
Continue with the next images...
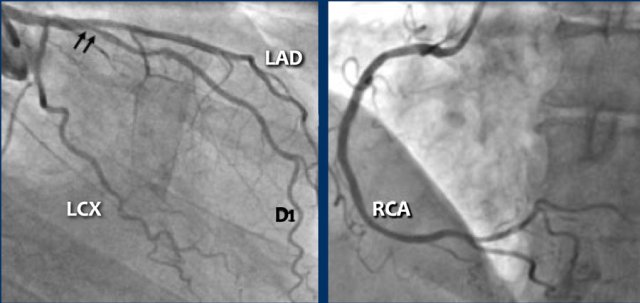
A: ICA correlates with CTA and shows an 80% stenosis in the mid LAD (white arrows) and a 60% stenosis in the D2 branch (black arrows). The D2 stenosis was overestimated on CTA.
B: PCI was performed during which a drug eluting stent (DES) was implanted with good results (white arrows).
case 4 - CAD-RADS 3/P1/I+ thrombus left ventricle
First, scroll through the CTA images.
How would you describe the findings on the coronary CTA?
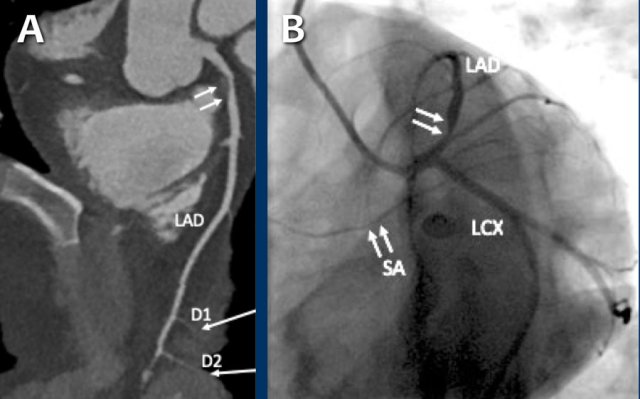
The findings are:
- Moderate (50-69%) stenosis in the proximal LAD caused by a non-calcified plaque.
- Variant of sinoatrial (SA) nodal artery. The artery usually arises from the RCA as a second branch after the conus artery, however in this case it arises from the LCX, courses behind the aorta, anastomosing with the right atrium and with a small branch supplies the SA-node of the heart.
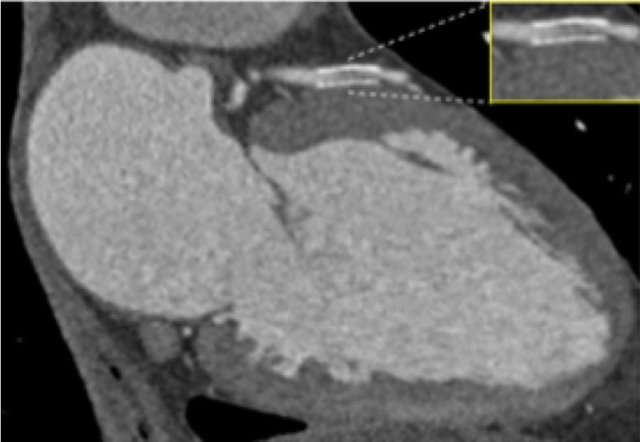
- Thrombus in the apex of the left ventricle.
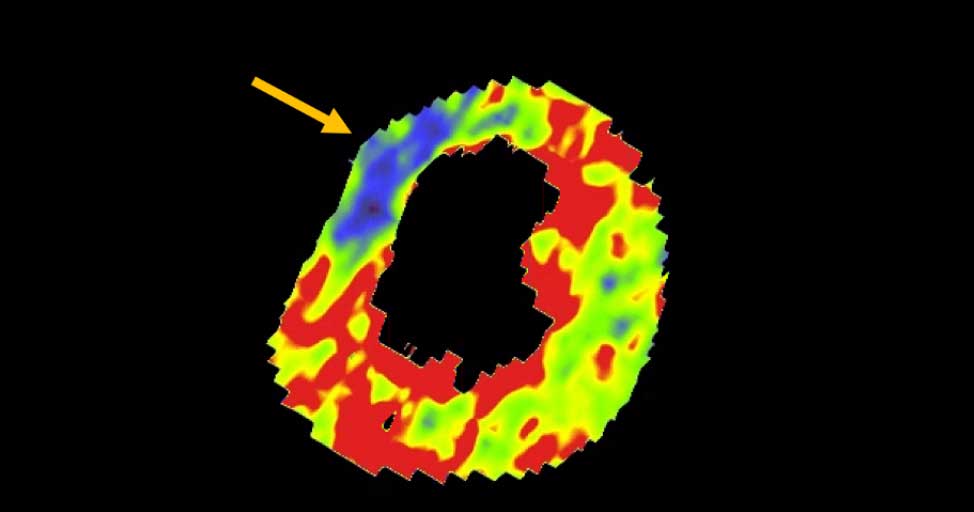
- CTP was performed in this patient. CTP showed a perfusion defect at stress imaging in the territory of the LAD (I+), at rest no perfusion defect was visible.
This patient classifies as CAD-RADS 3/P1/I+, which means
this patient requires further investigation.
...
Same patient.
A: Curved MPR of the LAD with non-calcified plaque causing moderate (50-69%) stenosis.
B: The so-called “spider-view” (LAO caudal) of the heart with a 70% stenosis in the proximal LAD. Note the presence of SA nodal artery arising from the proximal LCX and coursing to posterior direction.
C: A drug eluting stent (DES) was implanted into the proximal LAD with good results.
case 5 - CTA overestimates stenosis due to calcium
First, scroll through the CTA images.
How would you describe the findings on the coronary CTA?
Continue with the curved MPR images of the same patient.
The findings are:
- Long, partially
calcified plaque in the LM-LAD causing moderate stenosis (50-69%) (white
arrows).
This segment of the LAD is difficult to evaluate because of blooming and step artefacts. - Calcified plaque in the D1 causing severe stenosis (70-99%) at the origin (white arrows).
- Partially calcified
plaque proximal from the LCX stent with moderate (50-69%) stenosis (white
arrow).
LCX stent patent, no stenosis (black arrows). - Calcified plaques
in the proximal RCA with minimal stenosis (<25%) (white arrows).
RCA stent patent (black arrows).
Non-calcified plaque distal to the stent causing minimal stenosis (white arrowheads).
Another non-calcified plaque in the distal RCA causing minimal stenosis (<25%) (white arrows).
Partially calcified plaque in the distal RCA with mild stenosis (25-49%) (two white half-arrows). - Total plaque burden is extensive (P4).
Due to severe stenosis in D1, extensive plaque burden, some
non-diagnostic segments and a stent this patient classifies as CAD-RADS
4A/P4/N/S, which means that this patient needs further workup.
The ICA shows some wall irregularities to a maximum of 30% stenosis in
the proximal LAD.
The D1 shows 50% stenosis at the origin (black arrows). The LCX shows some wall
irregularities with no in-stent restenosis.
The RCA shows minimal wall irregularities, no in-stent restenosis.
This case also shows that CTA is limited in case of calcium and it can
overestimate the actual luminal stenosis.
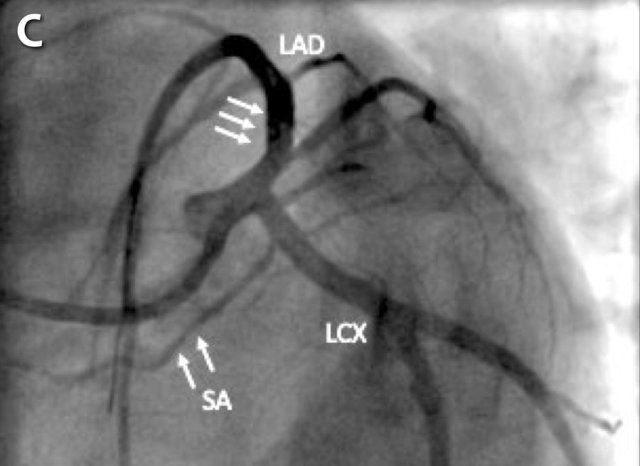
Continue with SPECT images of the same patient.
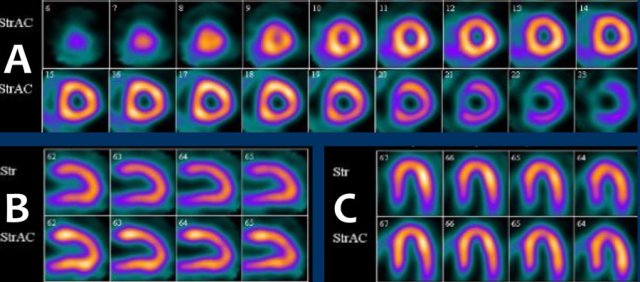 Myocardial SPECT attenuation corrected (AC) images during stress showing no perfusion defect. A: apex to base; B: septum to lateral wall; C: inferior to anterior
Myocardial SPECT attenuation corrected (AC) images during stress showing no perfusion defect. A: apex to base; B: septum to lateral wall; C: inferior to anterior
Shortly after the PCI the patient was again admitted with symptoms of
atypical angina.
SPECT myocardial perfusion was performed to exclude the presence of ischemia,
which showed no perfusion defect in the left ventricle.
The patient was treated with optimal medical care and no intervention was
performed.