Osteolytic - ill defined bone tumors
Henk Jan van der Woude and Robin Smithuis
Radiology department of the Onze Lieve Vrouwe Gasthuis, Amsterdam and the Rijnland hospital, Leiderdorp, the Netherlands
Publicationdate
In the article Bone Tumors - Differential diagnosis
we discussed a systematic approach to the differential diagnosis of bone tumors and tumor-like lesions.
In this article we will discuss the differential diagnosis of ill-defined osteolytic bone tumors in alphabetic order.
You can click on an item on the left.
Introduction
On the left the most common ill-defined bone tumors and tumor-like lesions.
An ill-defined zone of transition is seen in:
-
Malignant bone tumors:
- Ewing's sarcoma
- Osteosarcoma (most common presentation: sclerotic)
- Leukemia
- Metastases and Myeloma.
-
Aggressive benign lesions:
- Infection
- Eosinophilic granuloma
- locally aggressive Giant Cell Tumor
On the left a table with the most common bone tumors and tumor-like lesions in different age-groups.
In the middle column common ill-defined osteolytic lesions.
Notice the following:
- Infection is seen in all ages.
- ill-defined borders in GCT is seen in a locally aggressive lesion.
- Chondrosarcoma is usually well-defined, but high grade chondrosarcoma can be ill-defined.
- Metastases and myeloma are also usually well-defined, but sometimes ill-defined.
Chondrosarcoma
Key facts
- Most commonly presents as a well-defined lesion, but uncommonly it can be encountered as an ill-defined lytic lesion.
- Calcifications can be seen when there is a large myxoid component within the tumor, but they are not essential for the diagnosis.
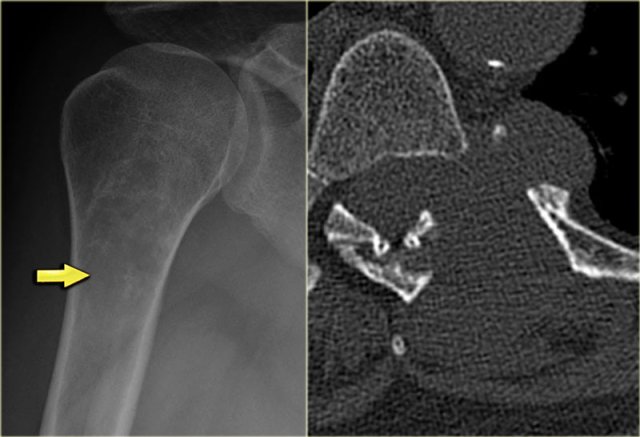
On the left a partially ill-defined osteolytic lesion with endosteal scalloping.
There are cloud-like calcifications indicating a chondroid matrix.
These imaging findings and the size of the lesion favor the diagnosis of a chondrosarcoma.
On the left two other lesions that proved to be a chondrosarcoma.
Notice that calcifications are not essential in chondrosarcoma.
On the left a lobulated partially ill-defined lytic lesion of the proximal humerus.
The presence of calcifications suggest that this is a chondroid tumor.
The lytic parts with cortical involvement and expansion should raise the suspicion of a high grade chondrosarcoma.
Eosinophilic granuloma
Key facts
- EG is like osteomyelitis a great mimicker of benign and malignant bone tumors.
- Must be included in the differential diagnosis of almost any ill-defined osteolytic bone lesion in patients under the age of 30.
- May also present as a well-defined lesion.
- EG can be excluded in patients > 30 years.
- Commonly found in the skull, mandible, spine and long bones, but can occur anywhere.
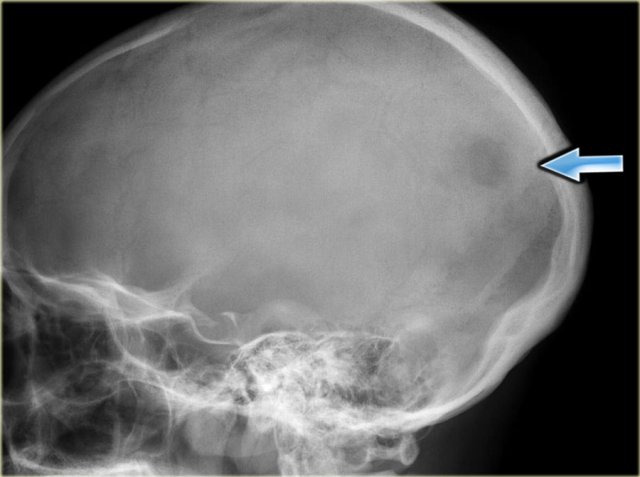
On the left some examples of EG with ill-defined borders.
There are single or multiple layered periosteal reactions.
On the left a typical presentation of EG in the skull as an ill-defined osteolytic lesion.
Ewing's sarcoma
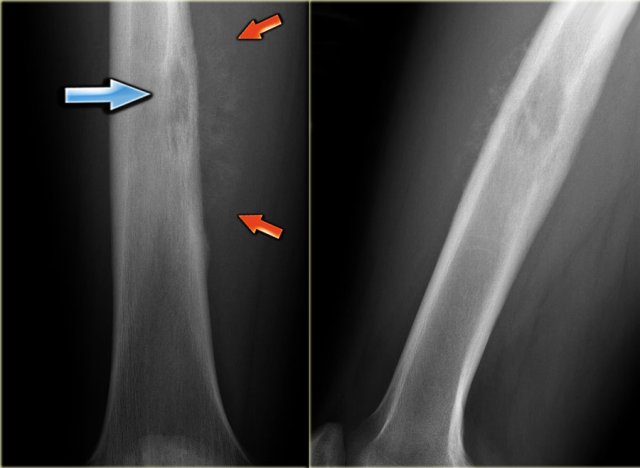 Ewing's sarcoma in diaphysis of the femur. Notice ill-defined zone of transition (blue arrow) and aggressive type of periosteal reaction (red arrows)
Ewing's sarcoma in diaphysis of the femur. Notice ill-defined zone of transition (blue arrow) and aggressive type of periosteal reaction (red arrows)
Key facts
- Most common presentation: ill-defined osteolytic lesion with multiple small holes in the diaphysis of a long bone in a child with a large soft tissue mass.
- Presentation with pain, mass, fever, anemia and leukocytosis.
- Most common location: femur, iliac bone, fibula, rib, tibia.
- Differential diagnosis: Osteosarcoma, lymphoma, infection and EG.
- Frequently aggressive type of periosteal reaction, but never a benign type.
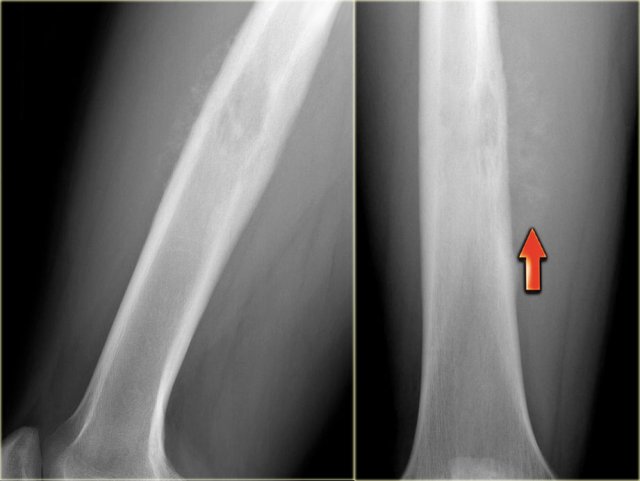
On the left a patient with a Ewing's sarcoma in the femur.
Notice the ill-defined osteolysis.
There is an aggressive periosteal reaction.
On the left an ill-defined lytic lesion in the femur of a young patient.
There is a permeative destruction pattern with irregular cortical destruction.
There is an aggressive periosteal reaction (arrow).
This is also called sunburst appearance.
On the left an ill-defined lytic lesion of the right iliac bone in a young patient which can easily be overlooked.
Final diagnosis: Ewing's sarcoma.
Giant cell tumor
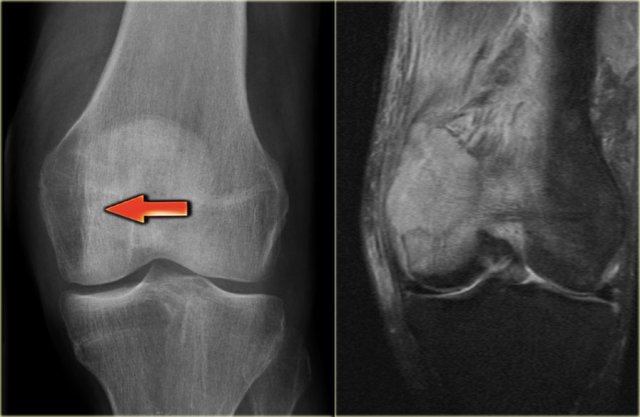
 GCT of the radius with ill-defined margins on the left and a GCT in the tibia with well-defined margins
GCT of the radius with ill-defined margins on the left and a GCT in the tibia with well-defined margins
Key facts
- Giant cell tumor is a benign lesion, but can be locally aggressive.
- A well-defined margin is associated with a locally less aggressive biologic behavior.
- In many cases the margin is ill-defined (figure).
- These tumors often thin the cortex and may expand into the soft tissues surrounding the bone.
- Most commonly seen in age 20-40 years. In the age group > 40 years, metastasis and plasmacytoma have to be included in the differential diagnosis.
On the left a giant cell tumor of the distal radius with ill-defined margins, destruction of the subchondral bone plate and extension towards the soft tissues.
On the right a giant cell tumor in the proximal tibia with somewhat better defined margin and non-interrupted cortical bone.
Lymphoma
Key facts
- Primary non-Hodgkin's lymphoma of bone is rare.
- Presentation: usually pain and palpable mass.
- Preferential sites: femur and humerus.
- Radiographic appearance may differ from virtually normal to severely permeative.
- Differential diagnosis:
- Ewing's sarcoma, however, lymphoma usually in higher age group
- Metastasis and plasmacytoma in age > 40y.
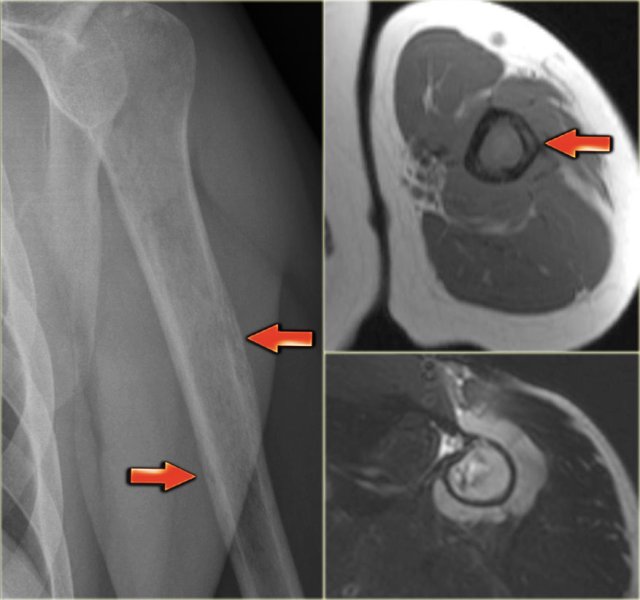
The plain radiograph on the left shows an ill-defined lytic lesion of the humerus diaphysis.
Notice tunneling of the cortical bone (red arrows).
On the MR notice the linear abnormalities within the cortical bone and the circumferential soft tissue mass.
Differential diagnosis (depending on age): Ewing's sarcoma, osteomyelitis and bone lymphoma.
Biopsy revealed Non-Hodgkin lymphoma
Metastases
Key facts
- Most common malignancy in bone.
- Must be considered in the differential diagnosis of any bone lesion in a patient > 40 years.
- May present as well-defined osteolytic, ill-defined osteolytic and also as sclerotic bone lesion.
- Majority of osteolytic metastases originate from breast, lung, kidney, colon, melanoma and thyroid.
On the left a 60 year old patient with a known malignancy.
There is a lesion in the distal femur, that you could easily overlook and think that it was focal osteopenia.
The lesion presents as a large ill-defined osteolytic mass extending into the epiphysis and almost abuttting the articular surface.
In a patient 20-40 years of age GCT would be a possible diagnosis.
It proved to be a metastasis.
Multiple Myeloma / Plasmacytoma
Key facts
- Multiple myeloma must be included in the differential diagnosis of any lytic bone lesion, either well-defined or ill-defined in age > 40.
- Most common presentation: multiple lytic 'punched out' lesions. A solitary presentation is referred to as plasmacytoma.
- Usually no increased uptake on bone scan.
- The most common location is in the axial skeleton (spine, skull, pelvis and ribs) and in the diaphysis of long bones (femur and humerus).
Osteomyelitis
Key facts
- Broad spectrum of radiographic features.
- May occur at any age, no typical location.
- Radiographic appearance: predominant reactive changes, including periosteal reaction, sclerosis and edema.
Periosteal reaction and permeative pattern may mimic malignant process: Ewing's sarcoma, osteosarcoma, lymphoma, leukemia. - In the pediatric age group eosinophilic granuloma may also mimic osteomyelitis.
- Pediatric osteomyelitis: most commonly in central metaphysis, may cross to epiphysis.
- Adult osteomyelitis: most commonly in central metaphysis or diaphysis.
- May be highly permeative with cortical breakthrough, abcesses and fluid along fascia on MR imaging.
On the left a subacute form of osteomyelitis.
There is an eccentric ill-defined lesion seen on both sides of the physeal plate in the proximal tibia.
This is highly suggestive for osteomyelitis.
Other lesions do not cross the growth plate in general.
On the right coronal T1-weighted MR image reveals a well-defined epi-metaphyseal lesion.
There is a dark peripheral zone of reactive sclerosis, and extensive edema with low signal Intensity in the metaphysis.
On the left an ill-defined osteolytic lesion in the proximal metaphysis of the tibia with extensive reactive sclerosis and solid periosteal reaction.
Osteosarcoma
Key facts of Osteosarcoma
- Hallmark of osteosarcoma is the production of bony matrix, which is reflected by the sclerosis seen on the radiograph.
- Usually typical malignant features including permeative-motheaten pattern of destruction, irregular cortical destruction and aggressive (interrupted) periosteal reaction.
- Occasionally an osteosarcoma may present as a lytic or mixed lytic-sclerotic lesion.
- Completely lytic osteosarcoma may represent telangiectatic subtype, composed of multiple cavities filled with blood (may resemble aneurysmal bone cyst!).
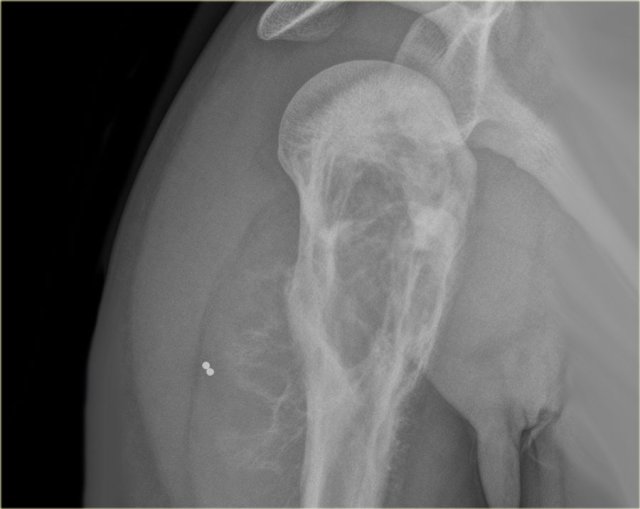
On the left a mixed osteolytic and sclerotic lesion in the proximal humerus with irregular cortical destruction.
There is an aggressive periosteal reaction and a soft tissue mass.