Cystic Abdominal Masses in Children
Erik Beek
Radiology department of the University Medical Center Utrecht in the Netherlands
Publicationdate
Cystic masses in the abdomen of a child are common.
Many of these are discovered with prenatal ultrasound.
Others are detected when a child has abdominal complaints and imaging is performed.
The cyst is either the cause of the complaints or an incidental finding.
In this pictorial essay we will show the most common abdominal cystic masses in children.
Ultrasound is often all that is needed for a diagnosis and will help the pediatrician or pediatric surgeon to make a treatment plan.
In difficult cases MRI and sometimes CT can be useful.
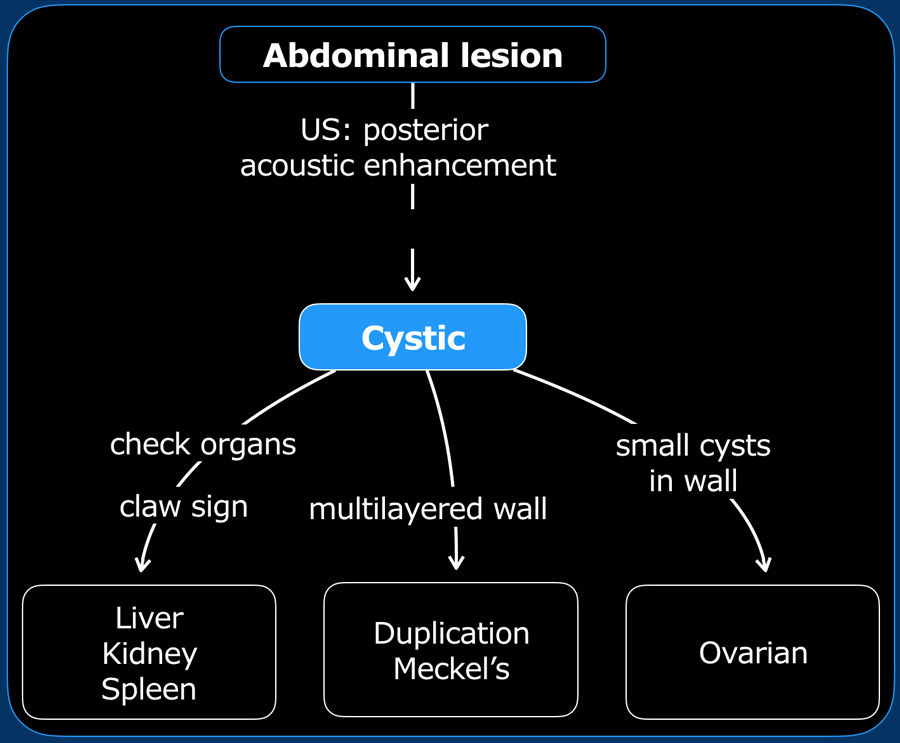
Systematic Approach
Differentiate cystic from solid
Ultrasound
Show posterior acoustic enhancement and edge shadowing artifact at the margins of the lesion.
Simple cysts are anechoic.
Hemorrhagic cysts may show diffuse internal echos and should not be confused with solid components.
MRI
MRI is more sensitive for diagnosing the solid nature of a lesion by demonstrating enhancement on T1W-images.
Be aware that fat and hemorrhagic components can demonstrate high T1 signal on pre-contrast images and should not be confused with enhancement of solid components.
Origin of lesion
Claw sign
This refers to the acute angles between lesion and parenchyma that indicates that this lesion has arisen from the parenchyma.
Check organs
Check liver, spleen, ductus choledochus, ovaries and pancreas. Normal ovaries excludes ovarian cysts.
Specific features
Small cyst in the wall of a lesion suggests ovarian origin.
Multilayered wall suggests origin from the digestive tract, e.g. duplication cyst or Meckels diverticulum
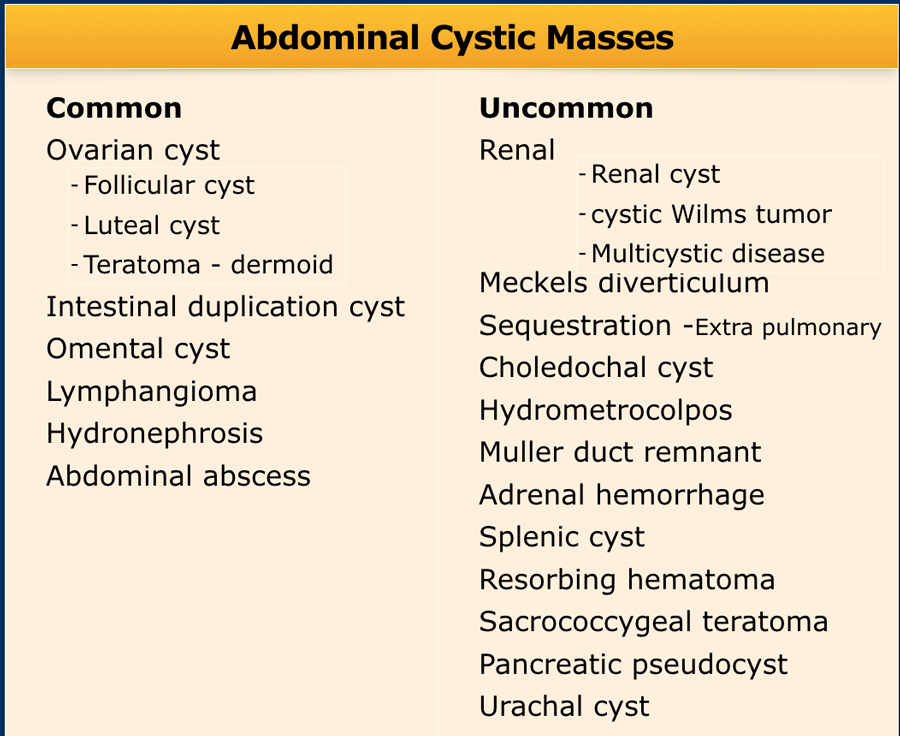
Differential diagnosis
The most common cystic lesions in the pediatric abdomen are listed in the table.
Rare cysts that we will not discuss are:
- Meconium cyst
- Hepatic cyst, hydatidic cyst, abscess
- Ectopic ureterocele
- Cerebral spinal fluid cyst with ventriculiperitoneal drain
- Appendical retention cyst/mucocele
- Anterior meningocele
- Other cystic malignancies
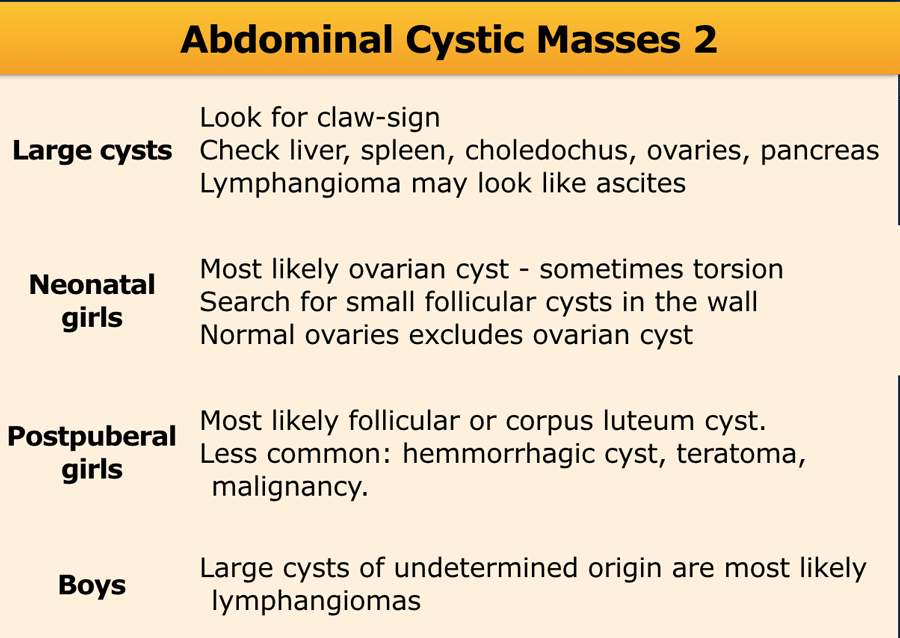
Large cysts
In large cysts it is often difficult to locate the origin. A "claw sign", an organ draped over a cyst, can help to pinpoint its origin. Look for the abdominal organs and try to establish if they are normal. In doing so, you can easily exclude cysts of the liver, spleen, kidneys, pancreas and choledochal duct.
Neonatal girls
In neonatal girls you are very likely dealing with an ovarian cyst.
Ovaries in young girls are very mobile and an ovary with a cyst can even be located at the liver hilum, so do not rely on its typical pelvic location.
Look at the wall of the cyst, search for small follicle cysts.
Only the depiction of two normal ovaries excludes an ovarian cyst, unless the cyst is clearly arising from some other organ.
Boys
In boys, large cystic lesions of undetermined origin are probably lymphangiomas.
These can be so large that they can be confused with ascites.
Look for sharp edged fluid in locations as Morrisons pouch or anterior to the liver to diagnose the fluid collection as ascites.
The content of a lymphangioma is often cloudy and looks like a "snow storm" when the cyst is compressed, while in ascites the content usually remains clear.
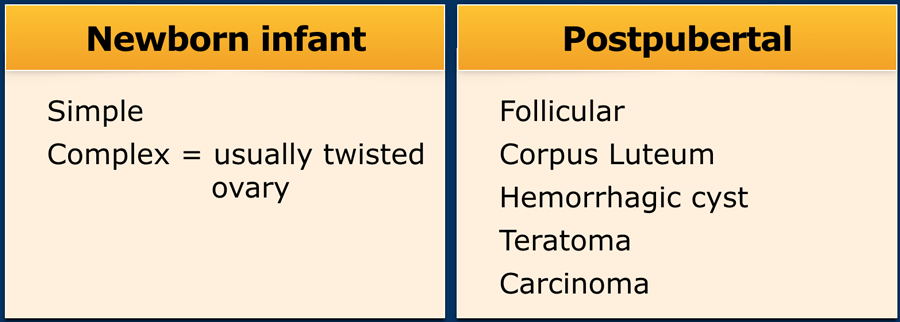
Ovarian cysts
Newborns and infants
With the introduction of prenatal ultrasound, ovarian cysts are often detected antenatally.
Ovarian cysts are divided in small (<4cm) or large cysts (>4 cm), and into simple, anechoic, thin-walled cysts or complicated cysts.
Complicated cysts are thick-walled, and can have debris and septa.
Most thick-walled cysts are twisted ovaries.
Some reports state that these will regress, but most are resected.
Postpubertal
The majority of ovarian cysts in postpuberal girls are functional cysts.
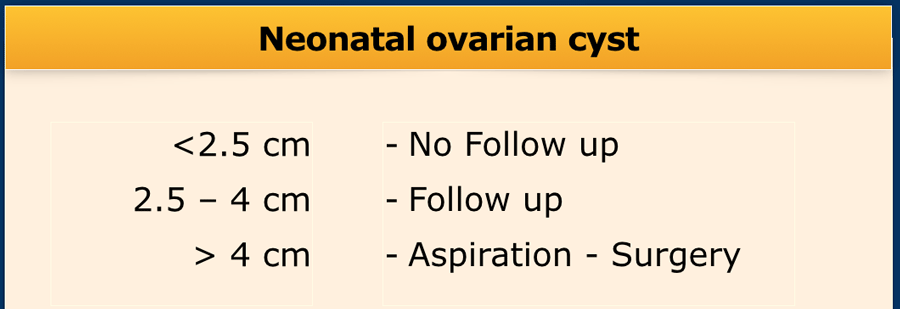
There are no strict guidelines for the management of ovarian cysts in infants.
Generally cysts >4 cm and complicated cysts are operated.
Cysts 2.5 - 4 cm are followed-up with US.
Cysts < 2,5 cm generally regress spontaneously over time and follow-up is not necessary.
Ovarian torsion
Suggestive features for ovarian torsion are:
- One-sided enlarged ovary with spherical cysts in the periphery.
- Commonly in midline location, above the uterus.
- The uterus is displaced towards the side of torsion.
- Often, there is an underlying ovarian lesions, e.g. teratoma.
- Whirlpool sign of a twisted vascular pedicle of the ovary. Be aware that Doppler findings in ovarian torsion can be widely variable. In contrast to the whirlpool sign of twisted vascular pedicle, that is highly specific for torsion.
- Fluid-debris level within the peripheral located cysts is pathognomic for ovarian torsion
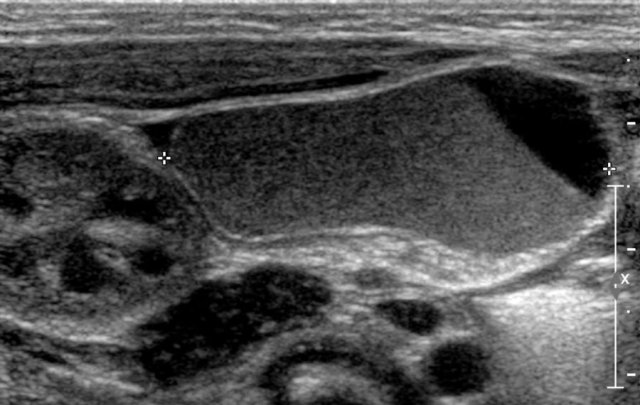
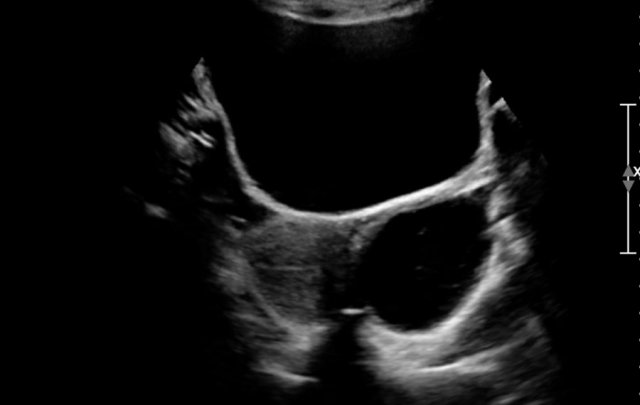
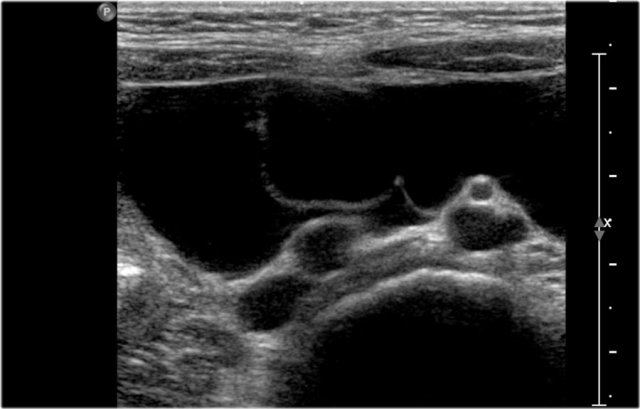
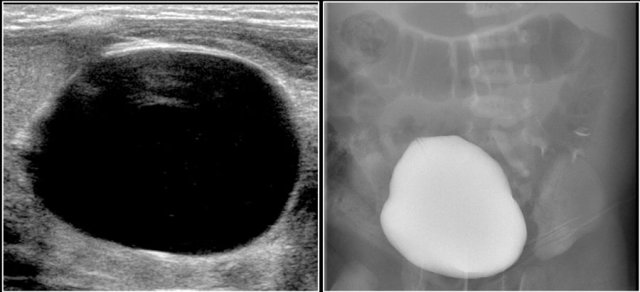
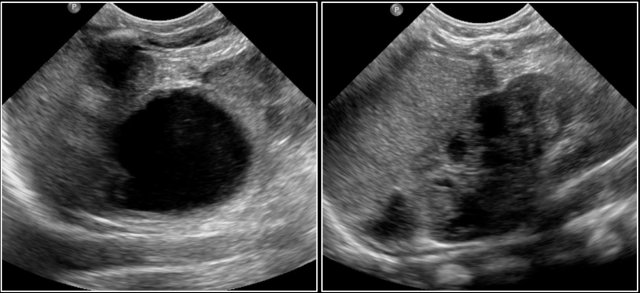
Here an antenatally detected cyst, confirmed after birth in a newborn girl.
A cyst with a fluid-fluid level is seen.
At operation a torsion of the left ovary was found.
Follicular cyst
The majority of ovarian cysts in postpuberal girls are functional cysts.
Normally several oocytes mature into follicles in a menstrual cycle. One of these becomes the dominant follicle, which ruptures and releases the oocyte. After release of the oocyte, the dominant follicle collapses, and the granulosa cells in the inner lining proliferate and swell to form the corpus luteum of menstruation.
Over the course of 14 days the corpus luteum degenerates, leaving the small scarred corpus albicans.
Read more...
So if one is thinking of a possible ovarian tumor process, do a follow-up ultrasound 2 weeks after the last menstruation day.
The lesion should be involuted in case of a corpus luteum cyst
Corpus luteum cyst
A corpus luteum may seal and fill with fluid or blood, forming a corpus luteum cyst.
The transvaginal ultrasound images show a small complex ovarian cyst with wall vascularity on power Doppler analysis.
The characteristic circular Doppler appearance is called the 'ring of fire'.
Note, there is good through-transmission and no internal vascularity, consistent with a, partially involuted, corpus luteum cyst.
Follow-up after one month demonstrated resorption of the mass and a normal left ovary.
Hemorrhagic ovarian cyst
When a Graafian follicle or follicular cyst bleeds, a complex hemorrhagic ovarian cyst (HOC) is formed.
On ultrasound an hemorrhagic ovarian cyst presents as an unilocular thin-walled cyst with fibrin-strands or low-level echoes and good through transmission.
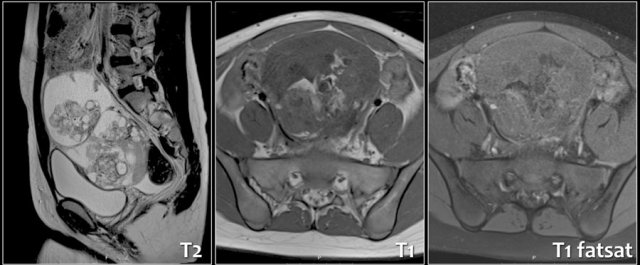
On MRI hemorrhagic cysts are bright on pre-contrast T1-FatSat, and dark on T2.
There should be no internal vascularity on Doppler ultrasound or post-contrast internal enhancement on CT or MRI.
Hemorrhagic ovarian cysts have variable wall thickness, and often some circumferential vascularity can be seen.
Clinically the classic presentation is with acute pain.
However HOC can also be an incidental finding in an asymptomatic patient.
Ovarian teratoma
Ovarian teratomas are composed of ecto-, meso-, and endoderm. They can become apparent as a large painless mass, but they can also twist, especially when the diameter is > 5 cm and cause an acute abdomen. Some are incidental findings.
On US a cystic mass can be seen with calcifications. Sometimes a fluid-fluid level is seen, by the separation of watery fluids and fat.
If the tumor contains lots of bone, hair, or calcifications, it is echogenic and sonographic diagnosis is challenging.
A Rokitansky nodule refers to a solid mass attached to the wall of a cyst, containing hair, bone, teeth or fat.
A plain abdominal film can sometimes show teeth or bone.
CT and especially MRI can provide a clear answer to the nature of the lesion.
On MRI some solid parts display high signal on T1, with low signal on fat suppressed sequences due to the fat content in the tumor.
Most of the solid parts enhance after Gadolineum.
Pathology demonstrated a immature teratoma.
The US- image shows a cystic lesion in the lower abdomen in a 3-year-old girl with colicky abdominal pain.
At operation a torsion of the right adnex was seen.
On pathology a teratoma was demonstrated.
Ovarian malignancy
Ovarian malignancies are rare.
The chance of malignancy is greater in younger girls (1-8 y) than in girls (15-19 y).
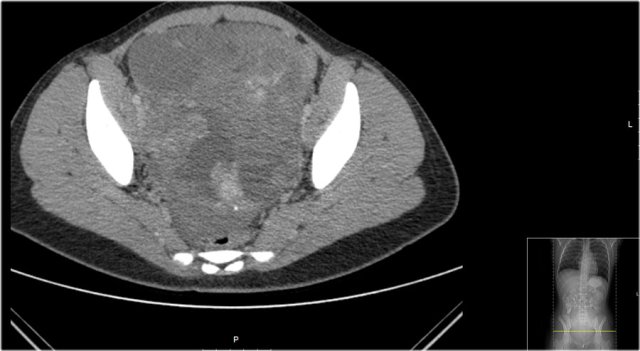
Here a CT-image of a 13-year-old girl presented with a lower abdominal mass.
It is a partly cystic, partly solid tumor with some calcifications.
The solid parts are inhomogeneous.
The tumor was resected and pathology showed a teratoma with malignant parts, with lymph node metastasis.
A mirror artefact of the bladder can mimick a cystic ovariumtumor.
When in doubt a repeat examination after emptying of the bladder will solve this problem.
Intestinal duplication cyst
Intestinal duplication cysts are duplications of the bowel.
The majority do not communicate with the bowel.
They can occur anywhere along the gastrointestinal tract.
The majority is in the jejunum and ileum. Most are on the mesenteric side and, if resected, a bowel resection is necessary. Intestinal duplication cysts present with bleeding, intussusception, obstruction, abdominal pain.
They can be found at prenatal ultrasound.
In typical cases a multilayered lining is seen, identical to a bowel wall and peristalsis may be visible.
If the cyst was infected the layers can be sloughed off. Ultrasound is usually sufficient to make the diagnosis.
Here an antenatally detected cyst in a girl.
Ultrasound showed a multilayered cyst and two normal ovaries.
At operation a duplication of the ileum was resected.
A six-month-old girl presented with vomiting.
Ultrasound demonstrated a multilayered cystic structure at the inner side of the duodenum. The cyst was partially resected, the common wall with the duodenum was left in situ.
Pathologic examination showed a duplication cyst.
Here an unusual appearance of a duplication cyst.
Ultrasound demonstrated an echogenic lesion in the left upper abdomen without a clear relationship to neighboring organs.
At operation a tumor of the mesentery was resected.
On macroscopic examination a tumor filled with a putty-like substance was seen.
On microscopic examination a duplication cyst of the jejunum was found.
Lymphangioma
 Large lymphangiomas can resemble ascites. Look for fluid anterior to the liver or in Morrisons pouch to exlude a lymphangioma.
Large lymphangiomas can resemble ascites. Look for fluid anterior to the liver or in Morrisons pouch to exlude a lymphangioma.
An abdominal lymphangioma consists of dilated lymphatic channels, comparable to the cystic lesions in the neck.
Sometimes the term omental cyst or mesenteric cyst is used.
On ultrasound cystic masses are seen, which can be clear or cloudy, unilocular or septated and small to very large.
In very large lesions with only a few septa the differentiation from ascites is difficult. Lymphangiomas do not creep into small spaces like ascites does, but they can be very soft with a plicated wall.
CT will demonstrate masses with water density.
Septa are less well seen than on ultrasound. After hemorrhage they can even appear solid.
The MRI characteristics depend on the absence or presence of bleeding or infection. Uncomplicated cysts are low on T1 and high on T2, but these signals are variable after bleeding.
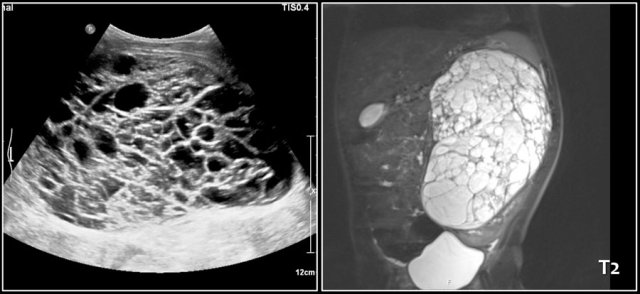
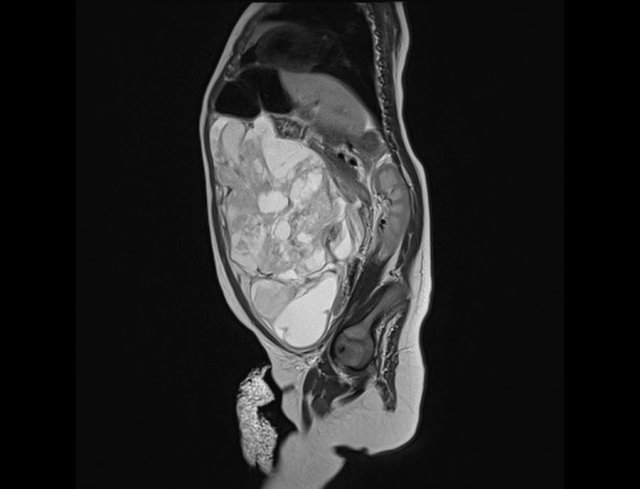
A one-year-old boy presented with a swollen abdomen.
A huge cystic lesion was seen with ultrasound, extending from the liver into the pelvis.
Some debris was visible.
A T2-weigthed coronal MR better shows the extension of the lesion.
At operation it was attached to the ascending colon, which was resected together with the lymphangioma.
Here a two-year-old boy with bilious vomiting.
Ultrasound showed a large thin-walled multicystic tumor, which appeared rather weak.
At operation a lymphangioma of the mesentery was resected.
Renal cystic masses
Renal cysts
Contrary to adults, simple renal cysts are rare in children.
Especially in young children think of a syndrome if you see renal cysts.
Cysts occur in tuberous sclerosis, von Hippel-Lindau syndrome, Zellweger syndrome, among others.
In children on dialysis the native kidneys will demonstrate cystic changes.
Autosomal dominant polycystic disease and autosomal recessive infantile polycystic disease are outside the scope of this article.
Hydronephrosis
A simple hydronephrosis of the kidney is easy to recognize.
It can be due to a ureteropelvic junction stenosis, ureteric stenosis or vesicoureteral reflux
If the hydronephrosis is huge it can be difficult to recognize as such, especially if debris is present.
It can mimic a dilated bowel loop, especially if it is accompanied by a tortuous dilated ureter full of debris with peristalsis.
A high frequency probe can show a thin layer of renal tissue surrounding the cystic structure.
Even a hugely dilated pelvicocalyceal system can turn out to be part of a well-functioning kidney.
Radionuclear examination or MRU, after nephrostomy, can provide information on the remaining renal function.
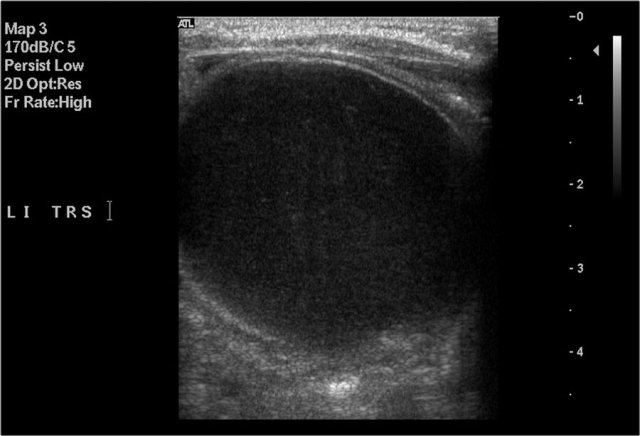
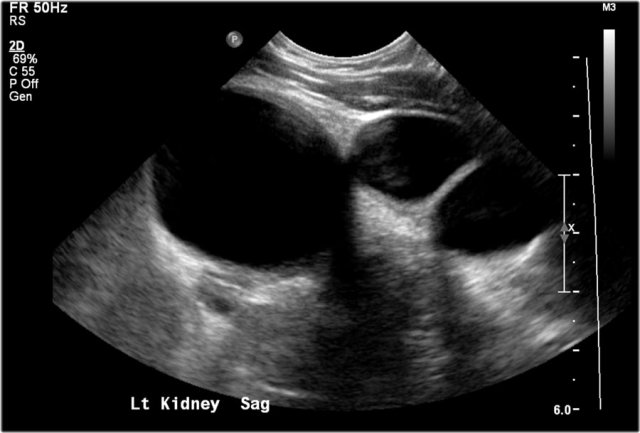
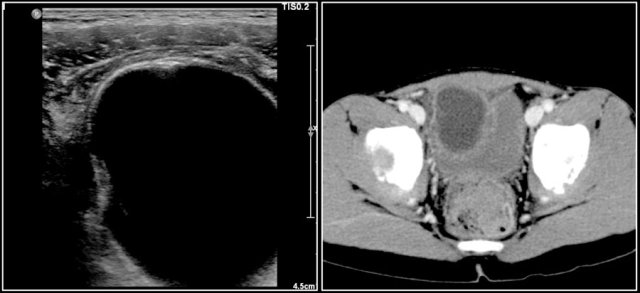
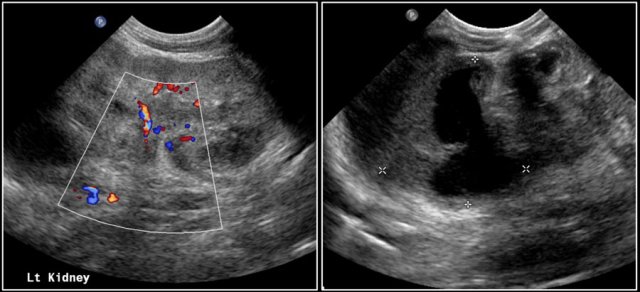
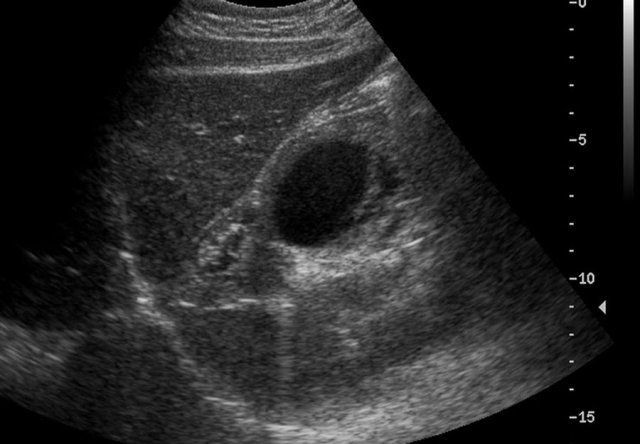
Here an ultrasound image of a five-month-old boy with an antenatally detected dilated pyelocalyceal system and no visible ureter, in accordance with a ureteropelvic junction stenosis.
On a sagittal image the dilated pyelocalyceal system is well seen.
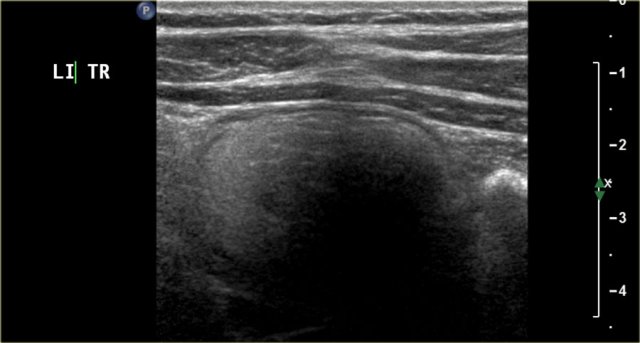
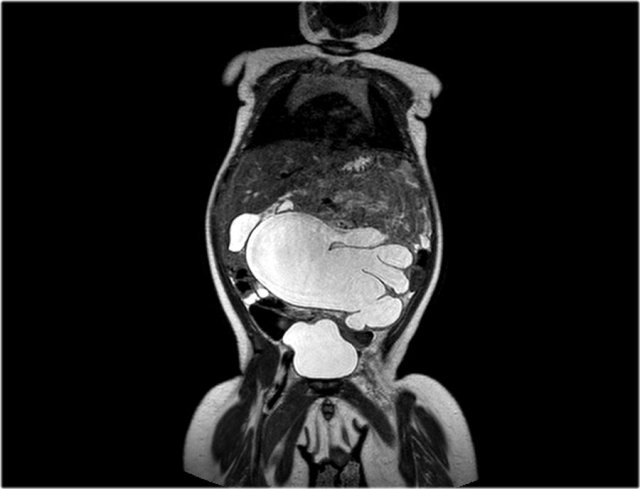
One-year-old boy was referred with a diagnosis of a cystic nephroblastoma.
Ultrasound detected a huge cyst in the middle of the abdomen.
When examined from the left flank with a high frequency linear array probe some parenchymal tissue was visible surrounding very dilated calyces. This is compatible with an extreme hydronephrosis.
At first it was thought that there were some solid parts in the cyst.
But when pressure was applied with the probe this proved to be debris.
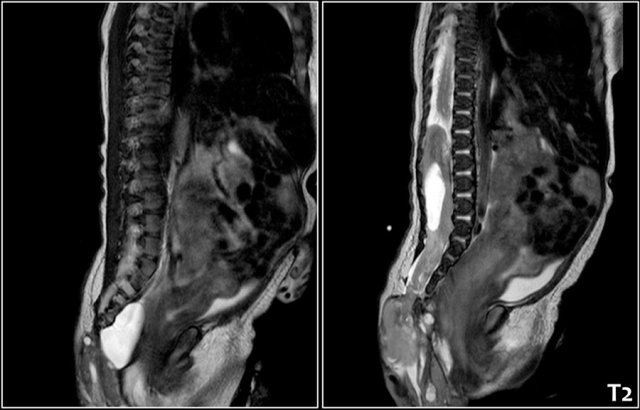
MRI depicts the hydronephrosis with more overview.
The cause was a pyeloureteric stenosis.
The left kidney had 33% split renal function on renography.
A pyelum reconstruction was successfully performed.
Multicystic kidney disease
A kidney, which is mainly composed of cysts of different sizes, is most likely a multicystic dysplastic kidney.
In multicystic dysplastic kidney there is no normal parenchyma and no ureter.
In approximately 25% of children with MCKD the contralateral kidney is affected by anomalies like reflux, ureteropelvic junction stenosis and positional abnormalities.
The majority of MCKD will regress in size over time.
Patients are followed with ultrasound to monitor the growth or involution of the MCKD and possible anomalies of the contralateral kidney.
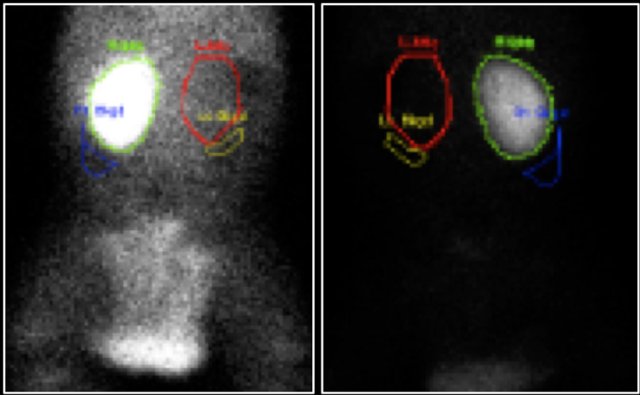
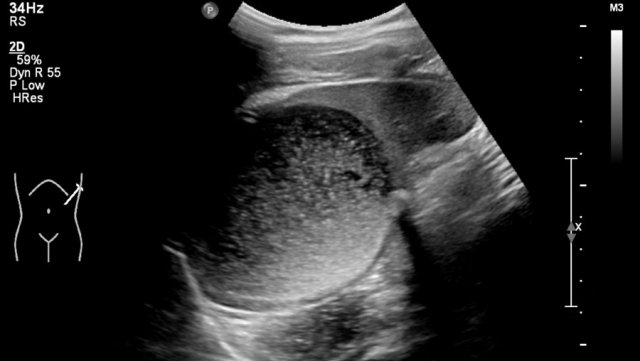
The image is of a one-month-old boy with a MCKD on prenatal ultrasound.
Some tissue and several large cysts are seen.
On Tc-99-DMSA scintigraphy no uptake was seen on the left side.
This is compatible with a MCKD.
Antenatally a duplex system of the left kidney was diagnosed with hydronephrosis. A postnatal ultrasound demonstrates a large cyst in the upper pole of the left kidney and some smaller cysts (not shown).
No normal parenchyma was visible.
On MCUG reflux in the lower pole system is seen, which is displaced caudally and rotated due to the upper pole mass.
This is probably a MCKD confined to the upper pole.
MCKD can affect one pole of a duplicated pelvicocalyceal system.
Cystic nephroma
Cystic nephroma consist of multiple cysts and septa and occur predominantly in young boys and older women.
These children present with an abdominal mass, or the tumor is found as an incidental finding during imaging.
A cystic nephroma can also be merely composed of cysts and look like a lymphangioma.
Especially in large tumors it can be difficult to visualize the remnants of the kidney from which the tumor stems.
A seven-year-old boy was examined after passing a kidney stone.
During ultrasound a multicystic tumor was detected.
An excision biopsy failed to remove the lesion.
During five years follow-up it was stable.
On MRI the lesion has a fuzzy demarcation and has water signal intensity on all pulse sequences.
The appearance is consistent with a cystic nephroma.
Nephroblastoma
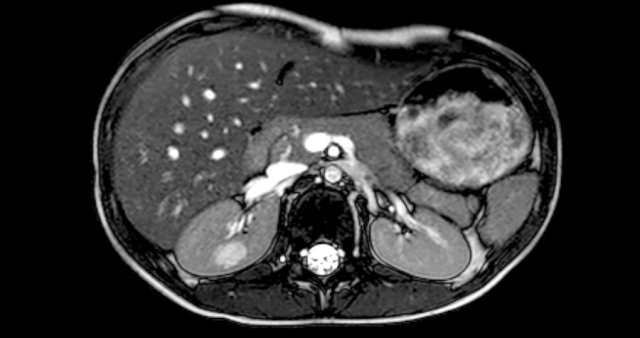
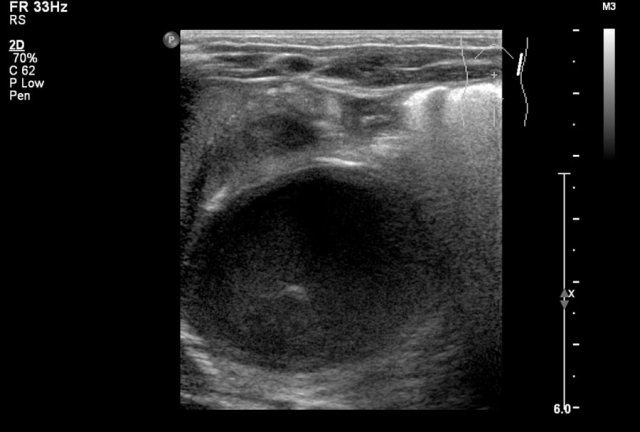
here an one and a half year old girl with a palpable tumor in the left abdomen.
Ultrasound showed a large tumor composed of innumerable cysts, originating from the left kidney.
On a T2 weighted coronal image the cysts are well displayed.
The remainder of the left kidney is at the caudal side of the tumor.
On pathology a cystic partially differentiated nephroblastoma was diagnosed.
Abdominal abscess
Abdominal abscesses can be seen after inflammation of abdominal organs, often appendicitis, and postoperatively. They are often of mixed echogenicity but can be largely cystic. The imaging strategy in children relies more on ultrasound then in adults, and during drainage procedures general anesthesia is often needed.
Meckels diverticulum
A Meckels diverticulum is a remnant of the omphalomesenteric duct, situated in the distal ileum. It can contain heterotopic remnants of gastric or pancreatic tissue. It is often asymptomatic and detected incidentally during operation.
Symptoms do occur, mostly in children below the age of two. It can present with intestinal bleeding, intussusception, or volvulus with obstruction. It can even mimic appendicitis.
Diagnosis can be made with technetium 99-m pertechnetate scintigraphy, depicting the ectopic gastric mucosa.
An inflamed Meckels diverticulum can be detected on ultrasound, but is easily misdiagnosed as an intussusception or appendiceal mass because it presents with a thickened bowel wall.
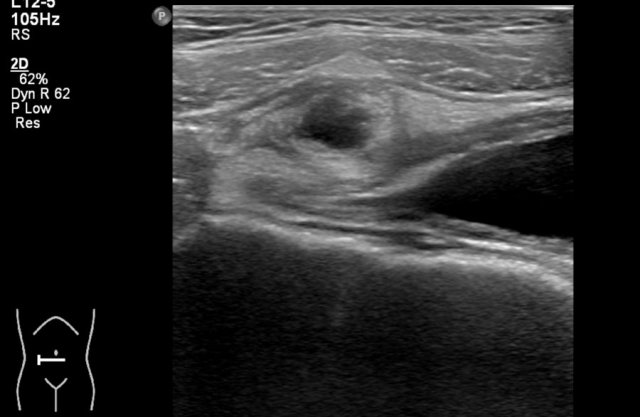
Nine-year-old boy with rectal bleeding.
At ultrasound a cystic structure was seen between the umbilicus and the bladder, with a multilayered wall.
This was diagnosed as eiither a Meckels diverticlum or a duplication cyst.
At operation a Meckels diverticlum was resected.
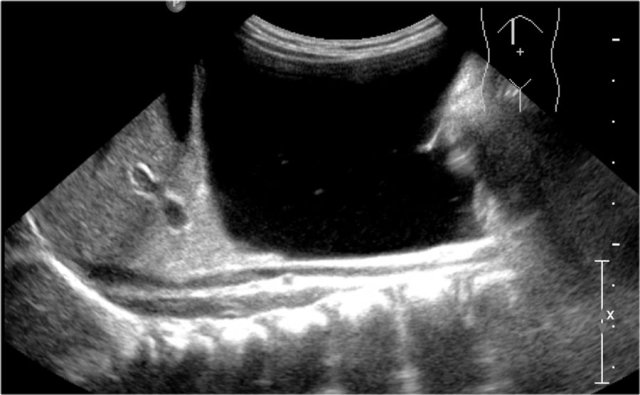
Nine-year-old boy with abdominal pain.
US and CT show a cystic structure with surrounding inflammation above the bladder. US demonstrated a multilayered wall.
The preoperative diagnosis was a Meckels diverticulum or duplication cyst.
At operation a Meckels diverticulum was resected.
Six-year-old girl presenting with acute intestinal obstruction.
Clinically an intussusception was suspected. Ultrasound showed a cystic lesion with a whirlpool sign, either a duplication cyst or a Meckels diverticulum.
At operation a Meckels diverticulum with adhesions and a volvulus was found.
Extrapulmonary sequestration
Extralobar pulmonary sequestrations can occur in the retroperitoneum, mostly on the left in a suprarenal position. They are usually detected on prenatal ultrasound as an echogenic mass. Cystic parts are commonly present. This lesion should be in the differential diagnosis of an adrenal hemorrhage or neuroblastoma.
Antenatally detected "shrunken third kidney". Postnatally a partly cystic, partly solid mass was seen in the left upper abdomen, separate from the spleen, kidney and adrenal gland. A presumptive diagnosis of a retroperitoneal sequestration was made. This was confirmed on pathology.
Choledochal cyst
Choledochal cyst is a rare anomaly. It classically presents with jaundice, a right upper abdominal mass, and abdominal pain. This triad is present in less than half of the patients.
A long common channel of the choledochal and pancreatic duct is thought to predispose to a choledochal cyst. Pancreatic juices are believed to reflux into the choledochal duct, causing an erosion of its wall.
The Todani classification is often used. (see diagram) Type 1 is the most common, followed by type 4.
Ultrasound can demonstrate these lesions. MRCP can support the diagnosis.
Choledochal cyst can be complicated by stone formation. If the stone is impacted it can cause bile duct dilatation and give the erroneous impression that type 4 is present instead of type 1.
Therapy is resection, because it is a precancerous disease.
Antenatally dectected cyst of the choledochal duct, confirmed on postnatal ultrasound as a Todani type 1 cyst. This was resected a few days after birth with a choledochojejunostomy and a Roux en Y loop
Hydrometrocolpos
If a vaginal septum persists the proximal vagina (colpos) and / or uterus (metros) can be dilated with fluid or blood, causing a hydrometrocolpos.
It occurs in two age groups: in neonatal girls in who it is often detected prenatally, and in pubertal girls in whom menstrual blood accumulates in the vagina.
It is caused by an imperforated hymen, or by a vaginal atresia of transverse vaginal septum.
It can be associated with renal agenesis. The kidneys should always be imaged in girls with genital anomalies.
Ultrasound can provide the right diagnosis. Anomalies of the uterus are better seen with MRI.
The differential diagnosis includes: Douglas abscess, rectal duplication, ovarian teratoma.
The video shows a large cloudy cyst in the lower abdomen, with a small uterus on top in a neonatal girl, consistent with a hydrocolpos.
Adrenal hemorrhage
Adrenal hemorrhage mostly occurs at birth. It presents at first as an echogenic mass, which slowly liquefies in the course of several weeks. Pediatricians can become restless if the liquefaction is late to occur, for fear of missing a neuroblastoma. Absence of flow and of calcifications favors a hemorrhage. Also decrease in size over time speaks for a hemorrhage.
If an adrenal hemorrhage has occurred antenatally the baby can be born with a cystic lesion, which can incidentally be detected. Sometimes a part of the adrenal gland is still visible with its characteristic multilayered texture. It can be confused with an obstructed upper pole moiety of a duplex kidney.
A left sided adrenal hemorrhage is associated with left renal vein thrombosis. The left adrenal vein connects to the left renal vein, contrary to the right adrenal vein, which connects to the inferior caval vein.
Like all hemorrhages an adrenal hemorrhage can be infected with formation of an abscess.
Two-day-old boy with delayed passage of meconium. On US an incidental finding of an cystic transformed adrenal hemorrhage, probably antenatally.
Two months later the lesion is resolving.
A newborn boy presented with hematuria. Ultrasound showed a left renal vein thrombosis with a swollen kidney and absent venous flow.
The left adrenal gland is enlarged and partly cystic, representing a left adrenal hemorrhage.
One-month-old girl with fever and an adrenal haemorrhage on the left. Infection of the haemorrhage was suspected. Aspiration yielded pus and a percutaneous drain was placed. The lesion resolved slowly.
Splenic cyst
Splenic cysts can be congenital or acquired, mostly posttraumatic. Congenital cysts are also named epithelial or epidermoid cysts.
Thick wall cyst can be considered as acquired, after trauma or after infection. They can be anechoic or contain debris. In smaller cysts the diagnosis is straightforward. In large cysts it can be difficult to determine the organ of origin.
Multiple cysts can be seen in lymphangiomatosis.
A 16-year-old girl underwent imaging for an ovarian tumor. As an incidental finding a splenic cyst with a lot of debris was seen. It is stable over the last four years.
Hematoma
Hematomas in the abdomen are generally echogenic at first presentation but in the resorption phase are often hypoechoic or anechoic and can present as a cystic mass. An adequate history will lead to the correct diagnosis.
Duodenal hematoma
A seven-year-old boy started vomiting a few hours after a duodenoscopy with biopsy. Ultrasound demonstrated a echogenic mass in the third part of the duodenum compatible with a hematoma.
After 6 weeks an anechoic lesion with some septa is seen
Fifteen-year-old girl with anorexia nervosa and signs and symptoms of a mild pancreatitis. Ultrasound demonstrated an echogenic cystic lesion below the pancreas against the duodenal wall. It looked like a hematoma.
At further history taking it turned out that the patient inflicted self-injury.
Teratoma
Sacrococcygeal teratoma
A sacrococcygeal teratoma is composed of solid tissue, cysts and calcifications. They are often detected at prenatal ultrasound and can be huge. There is a classification:
- Completely external, no presacral component
- External component and internal pelvic component
- External component and internal component extending into the abdomen
- Completely internal and no external component
Class 4 tumours can escape detection at birth and present later with constipation. The alpha-fetoprotein level will be elevated.
Diagnosis is generally made on physical examination and will be confirmed on ultrasound. An MRI is often made to document the exact extension of the tumor, especially to depict intraspinal extension, although ultrasound can demonstrate this as well in newborns and infants.
Two-year-old girl with a sacral mass. On ultrasound a cystic lesion anterior to the sacrum is seen, compatible with a class 4 sacrococcygeal teratoma. It was completely resected.
The intraspinal extension was visible on ultrasound, but MRI provides a better overview and a document for future comparison.
A parasagittal MRI shows a presacral cystic mass.
Newborn girl with a sacrococcygeal teratoma with external and internal solid and cystic parts, and a large intraspinal extension.
Teratoma of the gastric wall
Teratomas can be present in other locations than the ovary or the sacrococcyx. They will consist of cystic, solid and/or calcified parts. Their sonographic appearance is often confusing, as is their organ of origin. MRI is important here.
For-month-old boy with a large mass in the abdomen. Ultrasound shows a mixture of solid and cystic parts. It was separate from the solid abdominal organs.
MRI demonstrates the party cystic and partly solid mass. At operation a benign teratoma of the gastric wall was resected.
Pancreatic pseudocyst
A pancreatic pseudocyst is a fluid collection with a fibrous wall. It can occur after trauma to the pancreas or after pancreatitis, which is mostly seen after asparaginase therapy, especially used in leukemia treatment.
In older girls cystic tumors of the pancreas can occur. The most common is a solid pseuopapillary tumor.
Sixteen-year-old girl with a cystic lesion of the pancreatic tail. After excision pathologic examination showed a solid pseudopapillary tumor.
Urachal cyst
The urachus is a connection between the primitive bladder and the umbilical cord. If it does not obliterate several remnants are possible. The urachus can stay open, allowing urine to escape through the umbilicus. The most common remnant is a diverticulum on top of the bladder. It is also possible that a part of the urachus persists as a cyst in the course of the urachus.
Nine-year-old boy with right lower abdominal pain since 3 days. The boy was suspected to suffer from appendicitis but ultrasound showed a normal appendix and a inflames cyst above the bladder. After antibiotic treatment the lesion was excised. Pathologic examination showed a urothelium lined cyst, compatible with a urachal remnant.