Gallbladder wall thickening
Adriaan van Breda Vriesman, Robin Smithuis, Dries van Engelen and Julien Puylaert
Radiology Department of the Rijnland Hospital, Leiderdorp; the Groene Hart Hospital, Gouda and the Medical Centre Haaglanden, the Hague, the Netherlands
Publicationdate
Thickening of the gallbladder wall is a relatively frequent finding at diagnostic imaging studies.
Historically, a thick-walled gallbladder has been regarded as proof of primary gallbladder disease, and it is a well-known hallmark feature of acute cholecystitis.
The finding itself, however, is non-specific and can be found in a wide range of gallbladder diseases and extracholecystic pathological conditions.
In this review we discuss and illustrate the various causes of a generalized thickened gallbladder wall.
If you encounter printing problems with the margins of the document, try to adjust the margins or the scale of the document in the print settings.
Introduction
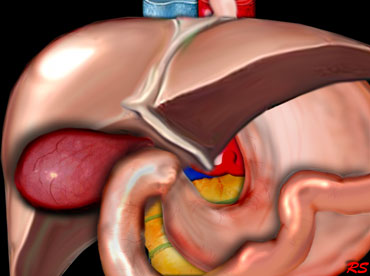 Distended hydropic and hyperemic gallbladder in acute cholecystitis due to stone obstruction in the gallbladder neck or cystic duct.
Distended hydropic and hyperemic gallbladder in acute cholecystitis due to stone obstruction in the gallbladder neck or cystic duct.
Sonography, CT and MRI all allow direct visualization of the normal and thickened gallbladder wall.
Traditionally, sonography is used as the initial imaging technique for evaluating patients with suspected gallbladder disease, because of its high sensitivity in the detection of gallbladder stones, its real-time character, speed and portability [1].
However, CT has become popular for evaluating the acute abdomen and often is the first modality to detect gallbladder wall thickening [2], or it may be used as an adjunct to an inconclusive sonography or for staging of disease.
The potential value of MRI in the evaluation of gallbladder pathology has been shown [3], but it still plays little role.
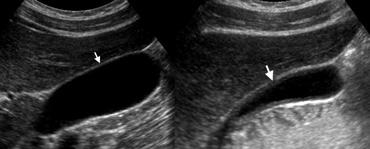 LEFT: US of a normal gallbladder after an overnight fast shows the wall as a pencil-thin echogenic line (arrow).RIGHT: US in the postprandial state shows pseudothickening of the gallbladder
LEFT: US of a normal gallbladder after an overnight fast shows the wall as a pencil-thin echogenic line (arrow).RIGHT: US in the postprandial state shows pseudothickening of the gallbladder
Normal gallbladder
The normal gallbladder wall appears as a pencil-thin echogenic line at sonography.
The thickness of the gallbladder wall depends on the degree of gallbladder distention and pseudothickening can occur in the postprandial state.
The normal gallbladder wall is usually perceptible at CT as a thin rim of soft-tissue density that enhances after contrast injection.
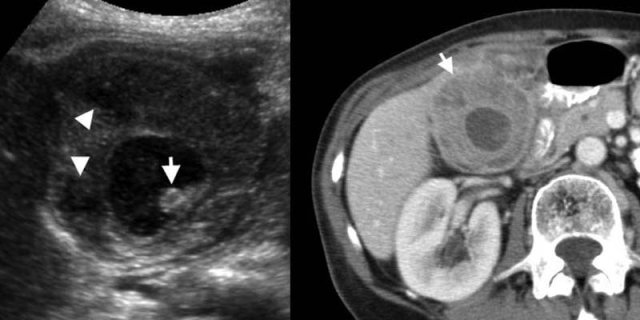
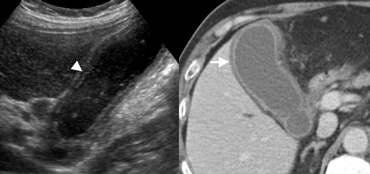 LEFT: US in a 59-year-old woman with acute cholecystitis shows the layered appearance of a thickened gallbladder wall, with a hypoechoic region between echogenic linesRIGHT: At contrast-enhanced CT the thick-walled gallbladder contains a hypodense outer layer (arrow) due to subserosal oedema
LEFT: US in a 59-year-old woman with acute cholecystitis shows the layered appearance of a thickened gallbladder wall, with a hypoechoic region between echogenic linesRIGHT: At contrast-enhanced CT the thick-walled gallbladder contains a hypodense outer layer (arrow) due to subserosal oedema
Thickened gallbladder wall
Thickening of the gallbladder wall is a relatively frequent finding at diagnostic imaging studies.
A thickened gallbladder wall measures more than 3 mm, typically has a layered appearance at sonography [1], and at CT frequently contains a hypodense layer of subserosal oedema that mimics pericholecystic fluid [2]
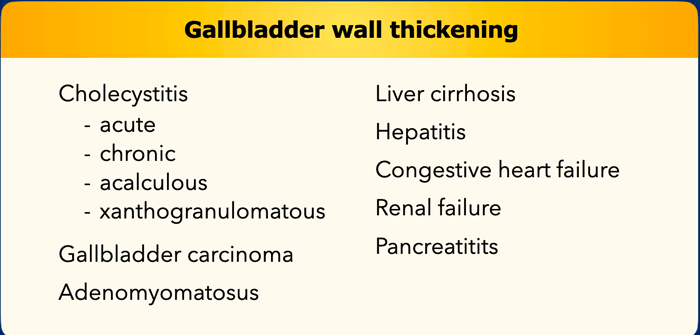
Differential diagnosis of gallbladder wall thickening
The differential diagnosis of gallbladder wall thickening is listed on the left.
Diffuse gallbladder wall thickening may produce a diagnostic problem, as it occurs in symptomatic and asymptomatic patients, and in patients with and without an indication for a cholecystectomy.
Diffuse thickening of the gallbladder wall may occur in patients who do not have a primary gallbladder disease, but in whom the gallbladder is secondarily involved in an extrinsic pathological condition.
In these patients a cholecystectomy is unwarranted, and gallbladder abnormalities will usually return to normal after correction of its extrinsic cause.
Primary gallbladder disease
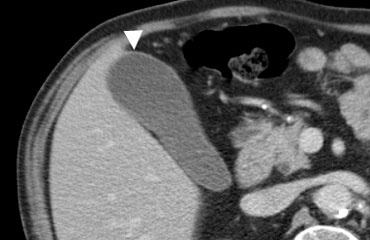
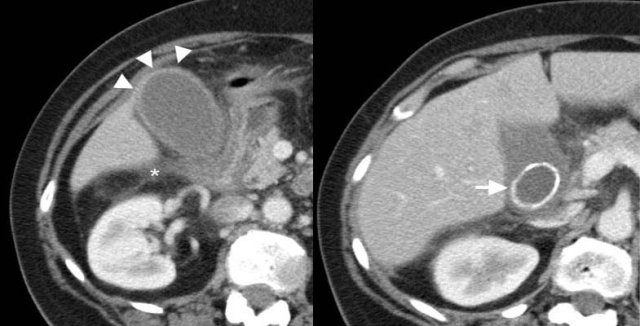 43-year-old woman with acute calculous cholecystitis. Contrast-enhanced CT shows a distended gallbladder (arrowheads) with a slightly thickened wall and subtle regional fat-stranding (asterisk). There is an impacted obstructing stone in the neck of the gallbladder (arrow).
43-year-old woman with acute calculous cholecystitis. Contrast-enhanced CT shows a distended gallbladder (arrowheads) with a slightly thickened wall and subtle regional fat-stranding (asterisk). There is an impacted obstructing stone in the neck of the gallbladder (arrow).
Acute cholecystitis
Acute cholecystitis is the fourth most common cause of hospital admissions for patients presenting with an acute abdomen [4], and it is the prime diagnostic concern when a thick-walled gallbladder is found at imaging.
This feature, however, is not pathognomonic for acute cholecystitis.
Additional imaging signs that support the diagnosis of acute calculous cholecystitis are:
- Obstructing gallstone
- Hydropical dilatation of the gallbladder
- Positive sonographic Murphy's sign ( i.e., pain elicited by pressure over the sonographically located gallbladder)
- Pericholecystic fat inflammation or fluid
- Hyperemia of the gallbladder wall at power Doppler.
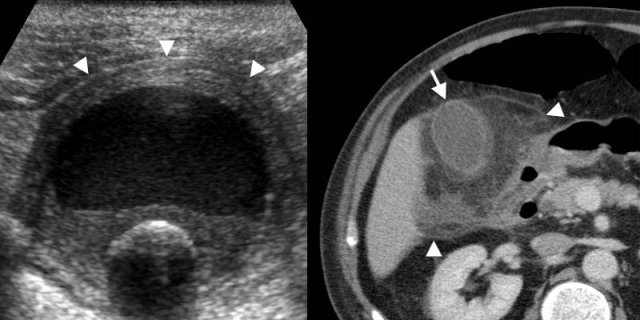
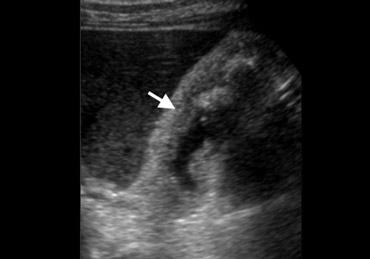
On the left images of a 62-year-old man with acute calculous cholecystitis.
Transverse sonogram at the spot of maximum tenderness shows a non-compressible hydropically distended thick-walled gallbladder (arrowheads), with an intraluminal stone and sludge or debris.
Contrast-enhanced CT depicts extensive fat inflammation (arrowheads) surrounding the
gallbladder (arrow).
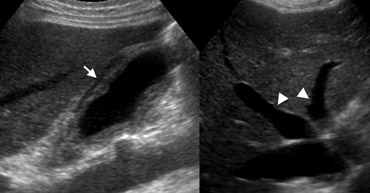
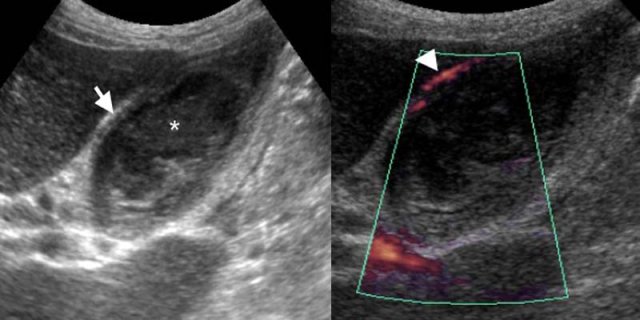 74-year-old man with acute acalculous cholecystitis. LEFT: US at the spot of maximum tenderness shows mural thickening of the gallbladder (arrow) that is completely filled with sludge (asterisk) without any stones. RIGHT: Power-Doppler sonography shows hypervascularity of the gallbladder wall (arrowhead), as a supporting sign of inflammation.
74-year-old man with acute acalculous cholecystitis. LEFT: US at the spot of maximum tenderness shows mural thickening of the gallbladder (arrow) that is completely filled with sludge (asterisk) without any stones. RIGHT: Power-Doppler sonography shows hypervascularity of the gallbladder wall (arrowhead), as a supporting sign of inflammation.
Acalculous cholecystitis
Acute acalculous cholecystitis mainly occurs in critically ill patients, presumably due to increased bile viscosity from fasting and medication that causes cholestasis.
The imaging features are those of acute cholecystitis, except for the absence of stones whereas gallbladder sludge is usually present (Fig).
Because in critically ill patients gallbladder abnormalities are frequently found secondary to systemic disease (see below), acalculous cholecystitis can be difficult to diagnose [5].
In these patients a percutaneous cholecystostomy can be both diagnostic and therapeutic.
 Chronic cholecystitis. Longitudinal sonogram of the gallbladder shows slight wall thickening (arrow) and an intraluminal non-obstructing stone
Chronic cholecystitis. Longitudinal sonogram of the gallbladder shows slight wall thickening (arrow) and an intraluminal non-obstructing stone
Chronic cholecystitis
Chronic cholecystitis is a term used clinically to refer to symptomatic gallbladder stones that cause transient obstruction, leading to a low-grade inflammation with fibrosis [1].
Correlation of the imaging finding of a stone-containing slightly thick-walled gallbladder with the clinical history is critical.
On the left images of a 49-year-old woman with chronic cholecystitis.
This patient had fasted overnight, so the wall-thickening does not represent physiologic contraction.
Correlation of these findings with her clinical history of recurrent colic-like right upper quadrant pain, due to transient gallbladder obstruction, is essential for the diagnosis.
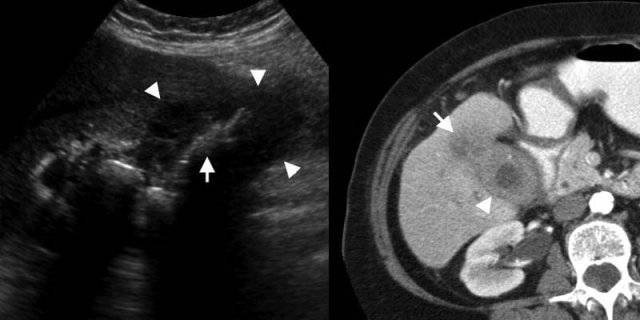
 Xanthogranulomatous cholecystitis. LEFT: US shows marked wall thickening with intramural hypoechoic nodules (arrowheads), and an intraluminal stone (arrow).RIGHT: Contrast-enhanced CT shows a deformed and thickened gallbladder wall containing hypoattenuating nodules
Xanthogranulomatous cholecystitis. LEFT: US shows marked wall thickening with intramural hypoechoic nodules (arrowheads), and an intraluminal stone (arrow).RIGHT: Contrast-enhanced CT shows a deformed and thickened gallbladder wall containing hypoattenuating nodules
Xanthogranulomatous cholecystitis
Xanthogranulomatous cholecystitis is an unusual variant of chronic cholecystitis, characterized by a lipid-laden inflammatory process comparable to xanthogranulomatous pyelonephritis.
Imaging studies show marked gallbladder wall thickening, often containing intramural nodules that are hypoechoic at sonography and hypoattenuating at CT, representing abscesses or foci of xanthogranulomatous inflammation.
These features overlap with those of gallbladder carcinoma, making preoperative distinction between these entities often impossible [6].
 Xanthogranulomatous cholecystitis. Hypoattenuating nodules ( arrowheads) represent abscesses. The lumen contains several stones (arrow).
Xanthogranulomatous cholecystitis. Hypoattenuating nodules ( arrowheads) represent abscesses. The lumen contains several stones (arrow).
On the left a 71-year-old man with xanthogranulomatous cholecystitis.
Contrast-enhanced CT shows a deformed and thickened gallbladder wall containing hypoattenuating nodules .
These represent abscesses or foci of inflammation.
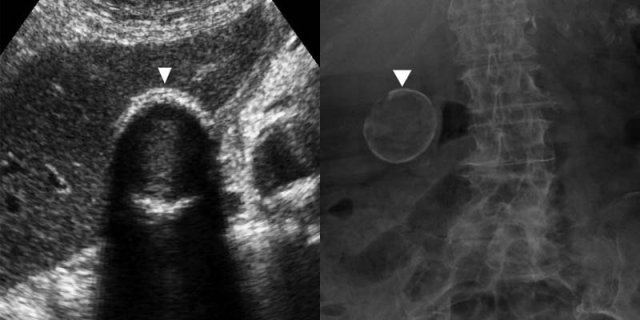
Porcelain gallbladder
A porcelain gallbladder is a rare disorder in which chronic cholecystitis produces mural calcification.
In these patients a prophylactic cholecystectomy has been advocated because of its association with gallbladder carcinoma [4]. However, this association appears to be weak.
 LEFT: Gallbladder carcinoma. US shows marked generalized wall thickening (arrowheads), replacing the gallbladder lumen. Multiple gallbladder stones (arrow) indicate the probable location of the filled lumen.RIGHT: Contrast-enhanced CT depicts a thick-walled gallbladder (arrowhead), with local infiltration of the mass in the adjacent liver (arrow).
LEFT: Gallbladder carcinoma. US shows marked generalized wall thickening (arrowheads), replacing the gallbladder lumen. Multiple gallbladder stones (arrow) indicate the probable location of the filled lumen.RIGHT: Contrast-enhanced CT depicts a thick-walled gallbladder (arrowhead), with local infiltration of the mass in the adjacent liver (arrow).
Gallbladder carcinoma
Gallbladder carcinoma is the fifth most common malignancy of the gastrointestinal tract, and is found incidentally in 1% to 3% of cholecystectomy specimens [4].
It is often detected at a late stage of the disease, due to lack of early or specific symptoms.
Gallbladder carcinoma has various imaging appearances, ranging from a polypoid intra-luminal lesion to an infiltrating mass replacing the gallbladder, and it may also present as diffuse mural thickening.
Associated findings such as invasion of adjacent structures, secondary bile duct dilatation, and liver or nodal metastases may help in differentiating a carcinoma from acute or xanthogranulomatous cholecystitis [2, 4].
In absence of these associated findings, it may not be possible to differentiate a carcinoma from xanthogranulomatous cholecystitis.
 Adenomyomatosis in a 39-year-old woman. US shows mural thickening with calcifications with the characteristic 'comet-tail' reverberation artifact (arrow) due to small cholesterol crystals within Rokitansky-Aschoff sinuses.
Adenomyomatosis in a 39-year-old woman. US shows mural thickening with calcifications with the characteristic 'comet-tail' reverberation artifact (arrow) due to small cholesterol crystals within Rokitansky-Aschoff sinuses.
Adenomyomatosis
Adenomyomatosis of the gallbladder is characterized by epithelial proliferation, muscular hypertrophia and intramural diverticula (Rokitansky-Aschoff sinuses), which may segmentally or diffusely involve of the gallbladder.
It is a benign condition that requires no specific treatment, occurring as an incidental finding in up to 9% of cholecystectomy specimens [6].
The sonographic finding of cholesterol crystals, shown as 'comet-tail'
reverberation artifacts (Fig), within a thickened wall of the gallbladder strongly suggests this diagnosis.
Air may produce a similar artifact, however, patients with emphysematous cholecystitis are usually ill in contrast to those with adenomyomatosis.
MR imaging may be able to differentiate adenomyomatosis from gallbladder carcinoma by depicting Rokitansky-Aschoff sinuses [7].
Secondary gallbladder involvement
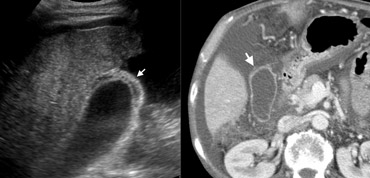 56-year-old man with liver cirrhosisLEFT: US depicts wall thickening (arrow), surrounded by ascites. Note the irregular cirrhotic liver parenchyma. RIGHT: At contrast-enhanced CT the wall of the gallbladder (arrow) appears nearly normal, because subserosal oedema can not be well differentiated from surrounding ascites at CT.
56-year-old man with liver cirrhosisLEFT: US depicts wall thickening (arrow), surrounded by ascites. Note the irregular cirrhotic liver parenchyma. RIGHT: At contrast-enhanced CT the wall of the gallbladder (arrow) appears nearly normal, because subserosal oedema can not be well differentiated from surrounding ascites at CT.
Liver cirrhosis
Systemic diseases such as hepatic dysfunction, heart failure, or renal failure may lead to diffuse gallbladder thickening [1, 2].
The exact pathophysiologic mechanism leading to oedema of the gallbladder wall in these diverse conditions is uncertain, but it is likely due to elevated portal venous pressure, elevated systemic venous pressure, decreased intravascular osmotic pressure, or a combination of these factors.
Hypoproteinemia has also been reported as a cause of extrinsic gallbladder disease, but this has been disputed [8].
Liver cirrhosis, hepatitis and congestive right heart failure are relatively frequent causes.
The case on the left is a patient with liver cirrhosis.
The secondary gallbladder wall thickening is presumably due to elevated portal venous pressure and decreased intravascular osmotic pressure.
Hepatitis
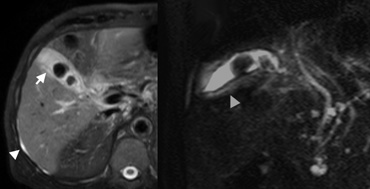
On the left a 75-year-old man with drug-induced hepatitis.
Longitudinal sonogram of a non-distended gallbladder shows diffuse wall thickening (arrow), and incidental cholelithiasis which may be confusing.
In the same patient with the drug-induced hepatitis MR images were obtained to evaluate the bile ducts because of abnormal liver function tests.
On the far left Axial SPIR T2-weighted image (A) shows a small amount of ascites (arrowhead) which indicates that the thickened gallbladder wall (arrow) probably has an extrinsic systemic cause.
Next to it an oblique HASTE image for MR cholangiography that excludes choledocholithiasis.
Mural thickening of the gallbladder (arrowhead) is also shown.
Congestive right heart failure
On the left a 74-year-old man with congestive right heart failure.
Ultrasound depicts diffuse wall thickening of a stone-free painless gallbladder and large-caliber hepatic veins (arrowheads) and inferior vena cava, as supporting evidence of right heart failure.
 Pancreatitis in a 56-year-old man Contrast-enhanced CT shows peripancreatic inflammatory changes (arrowheads), and thickening of the wall of the gallbladder (arrow) which is secondarily involved in the pancreatic inflammation.
Pancreatitis in a 56-year-old man Contrast-enhanced CT shows peripancreatic inflammatory changes (arrowheads), and thickening of the wall of the gallbladder (arrow) which is secondarily involved in the pancreatic inflammation.
Pancreatitis
Extracholecystic inflammation may secondarily involve the gallbladder causing wall thickening, due to direct spread of the primary inflammation, or less frequently due to an immunologic reaction [8].
Theoretically, it may be caused by any inflammation that extends to the region of the gallbladder, but only few are regularly encountered including hepatitis, pancreatitis (Figure), and pyelonephritis.
Gallbladder wall thickening has also been reported in patients with infectious mononucleosis [9], and in patients with AIDS due to opportunistic infections or secondary neoplastic infiltration [2].
Conclusion
Diffuse gallbladder wall thickening can result from a broad spectrum of pathological conditions, including surgical and non-surgical diseases.
At times a definite imaging diagnosis may be impossible.
In most cases however, the cause can be determined by correlation of the associated imaging findings with the clinical presentation.
Charity
All the profits of the Radiology Assistant go to Medical Action Myanmar which is run by Dr. Nini Tun and Dr. Frank Smithuis sr, who is a professor at Oxford university and happens to be the brother of Robin Smithuis.
Click here or on the image below to watch the video of Medical Action Myanmar and if you like the Radiology Assistant, please support Medical Action Myanmar with a small gift.