Acute Abdomen in Gynaecology - Ultrasound
Julien Puylaert
Amsterdam UMC and Haaglanden MC, The Hague
Publicationdate
This is a pictorial essay of the various gynaecological conditions that may cause acute abdominal pain, as far as they are encountered in daily radiological practice.
Conditions which present
during a known pregnancy like
miscarriage, early ectopic pregnancy, uterine rupture and placental abruption, as well as puerperal endometritis,
are not included as they belong to the professional terrain
of the gynaecologist.
These conditions are rarely seen in the daily radiological practice of acute
abdomen.
For critical comments and additional remarks: j.puylaert@gmail.com
Introduction
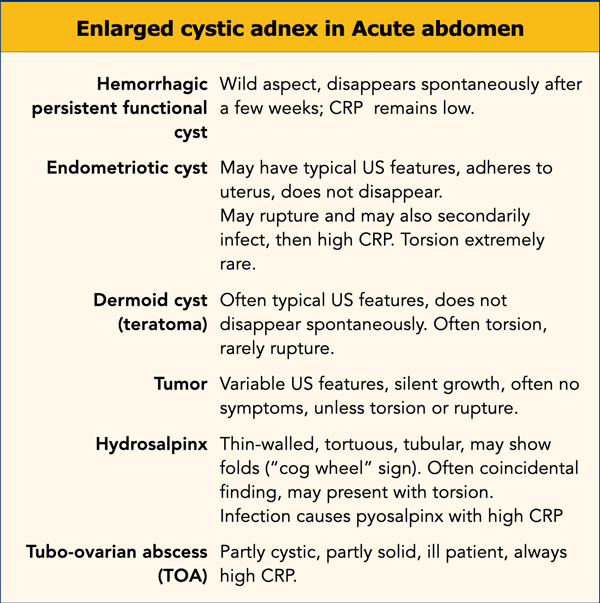
This table summarizes the gynaecological diseases that may present
with acute abdominal pain.
It is divided into pathology in:
- Pregnant women
- Women in the post-partum period
- Non-pregnant women
Normal US anatomy
Uterus and ovaries are best visualized with the bladder half-full.
A very full bladder is unpleasant for the patient, hampers adequate compression and pushes organs away from the ventral abdominal wall, excluding the use of high frequency probes.
In the sagittal view the uterus, cervix, vagina, anorectum and urethra (u.) can be identified, as well as the collapsed anterior and posterior fornix of the vagina.
Studying a uterus, which is in retroflexion, requires more bladder filling.
Transverse view allows visualization of both uterus and ovaries.
The uterus itself may also provide an acoustic window to visualize the ovaries.
With the uterus in anteflexion, the ovaries are quite ventrally localized and can often be visualized using the right and left iliac vessels as an acoustic window (figure).
Dominant follicle
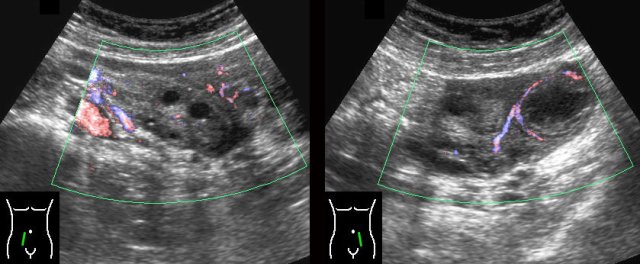
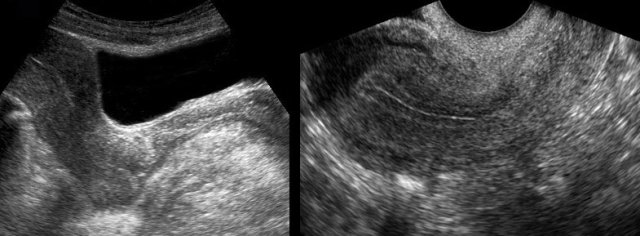
In women of the fertile age the normal inactive ovaries show moderate vascularization (left image).
During the pre-ovulatory phase the dominant follicle can be identified by its “ring-of-fire” (right image).
Luteal body
After the ovulation the dominant follicle becomes smaller (left) and in the absence of pregnancy, turns into a crenulated luteal body (right).
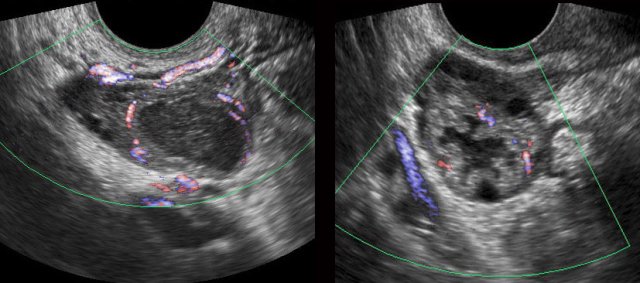
Transvaginal ultrasound (TVUS) has great advantages in visualizing the uterus and ovaries.
It can also be used for non-gynaecological conditions such as appendicitis, diverticulitis, etc.
The use of transvaginal ultrasound will be dealt with in a different article: TVUS for non-gynaecological conditions.
Acute gynaecological conditions in pregnancy
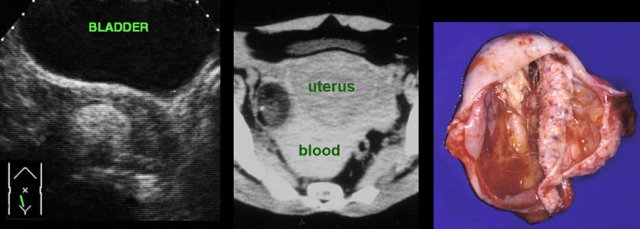
Ectopic pregnancy
The most important cause of acute abdominal pain in pregnant women is ectopic pregnancy.
Therefore in every woman of the fertile age group with acute abdominal pain, β-hCG levels are determined.
The US hallmark of an ectopic pregnancy is the combination of elevated β-hCG levels in serum or urine, with an empty uterus.
There
are however many pitfalls, especially in early ectopic pregnancy.
Small intracavitary fluid collections and thickened endometrium may lead to the erroneous diagnosis of an intra-uterine pregnancy.
On the other hand, a very early intra-uterine
pregnancy may not yet be visible at US.
All
these pitfalls belong to the exclusive terrain of the gynaecologist and will
not be discussed here.
Pregnancy
may be unknown to clinician and patient, and an ectopic pregnancy may present
with atypical symptoms.
In such cases, the radiologist can be confronted with an
unexpected ectopic pregnancy and must be aware of the US findings.
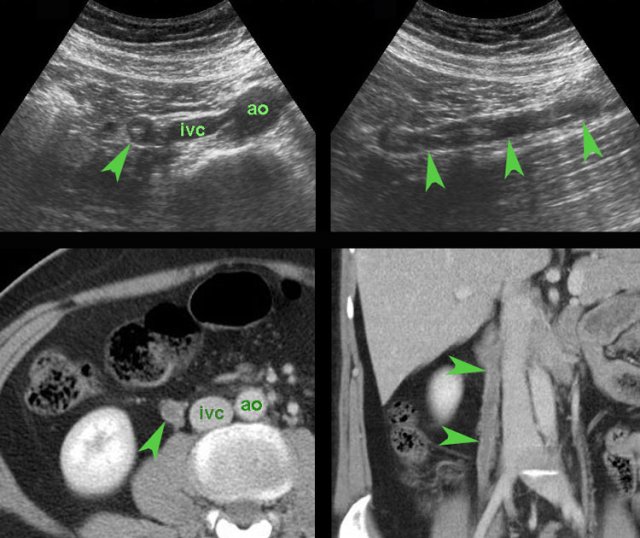
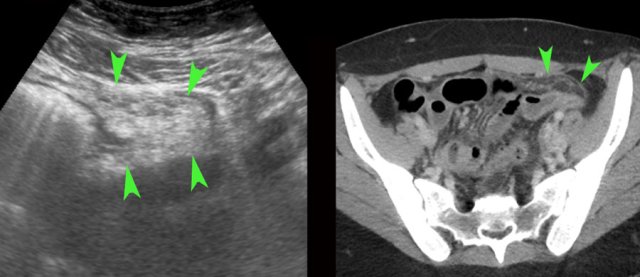
case 1
This
48 year old woman presented with appendicitis-like symptoms and was unaware of being
pregnant.
US showed a large heterogeneous, avascular mass (arrowheads) to the right and dorsal of the uterus, suspect for a
large blood clot.
There was also some liquified blood higher up (*).
Subsequently performed pregnancy test was positive, and laparoscopy confirmed a ruptured tubal pregnancy.
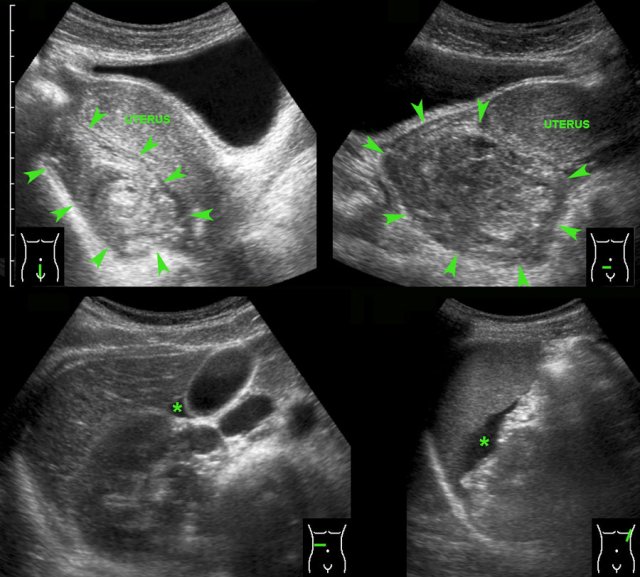
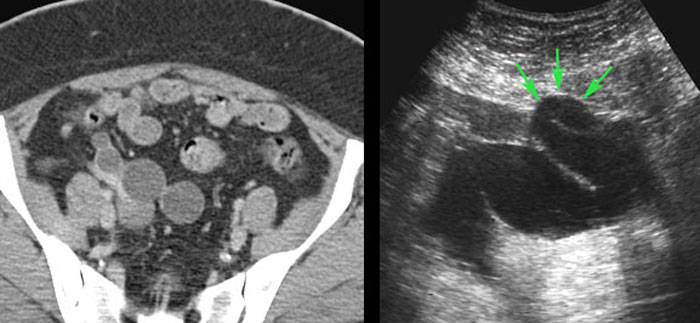
case 2
In this patient submitted for suspected stomach perforation, a large inhomogeneous mass of blood clot (arrowheads) in the left peritoneal cavity was visualized (right upper image).
Such a
large clot can easily be mistaken for normal mesenterial fat or bowel.
Awareness
and careful inspection of this mass, which lacks peristaltic movements, are helpful findings to differentiate.
This patient had also a lot of free fluid, which at puncture was liquified blood (right lower image).
Laparoscopy demonstrated 1.5 liter of blood and a ruptured tubal pregnancy.
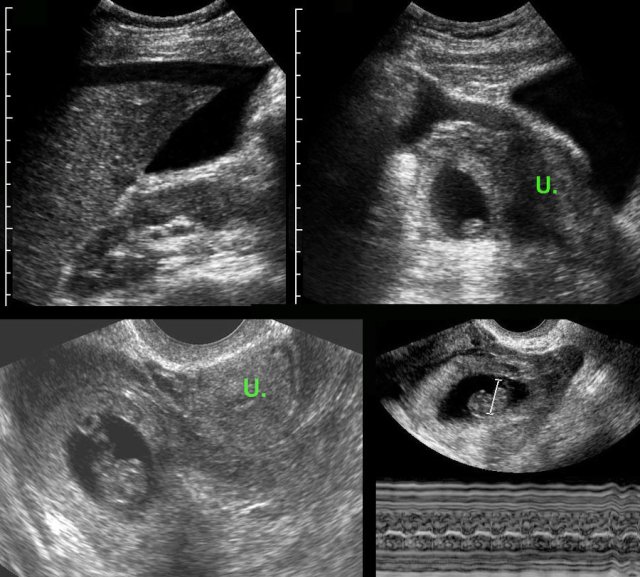
case 3
This patient was submitted for suspected perforated appendicitis.
US showed free fluid and to the right of the uterus (U.), a gestational sac containing a living fetus.
Fetal heartbeat was documented by TVUS with M-mode (right lower image).
A living fetus is found in less than 10 % of all ectopic pregnancies.
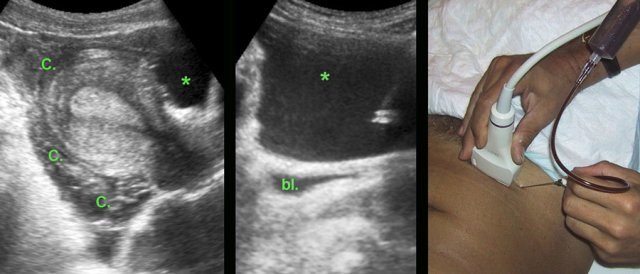
case 4
Luteal body bleeding mimicking an ectopic pregnancy
In
this young woman, US demonstrated a large quantity of clotted (C.) and liquified
blood (*) around the uterus, suspect for ectopic pregnancy. However, β-HCG levels in both urine and serum were extremely
low.
US guided puncture in the liquified part confirmed blood. (bl. = bladder)
Laparoscopy revealed severe bleeding from a luteal body, which was successfully coagulated.
Ischemic myoma
During pregnancy a myoma may increase in size and outgrow its vascularization.
case 1
This 25 year old pregnant woman presented with a palpable, painful mass in the RLQ, suspect for an “appendiceal mass”.
US revealed a hypoechoic, inhomogeneous, hypovascular round solid mass arising from the myometrium, and “bulging” into the abdominal wall during compression.
The
diagnosis was an ischemic myoma.
She was successfully treated
with analgesics.
Labor inhibitors were not
necessary.
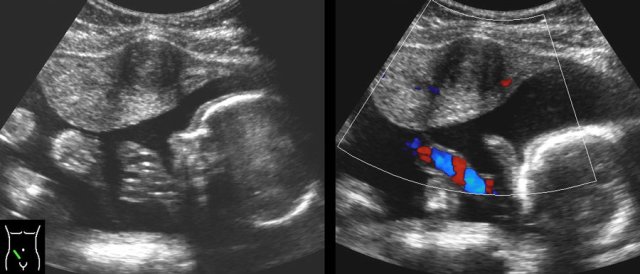
case 2
Here another case of an ischemic myoma.
The extrinsic location in this case suggests that this is a
pedunculated myoma (arrowheads).
This patient was successfully treated with analgesics and labor inhibitors.
Torsion of enlarged adnex
Adnexal torsion causes sudden, severe pelvic pain.
Risk factors for adnexal torsion include pregnancy, induction of ovulation and ovarian enlargement to > 4 cm (particularly by cysts or benign tumors).
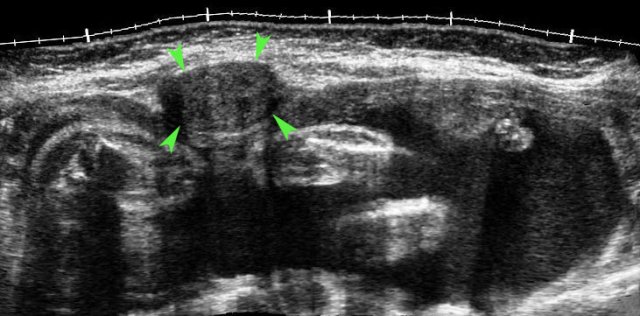
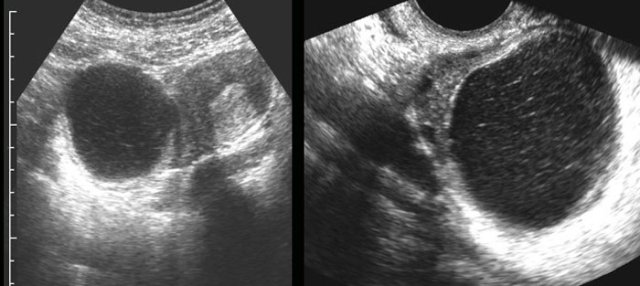
case 1
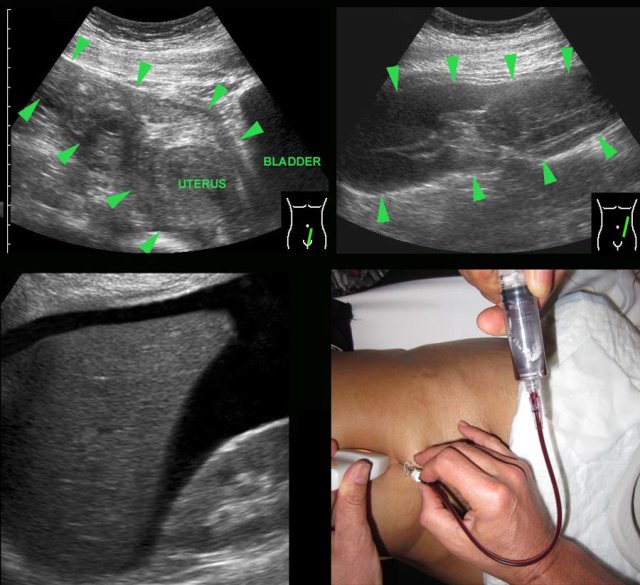
This pregnant
patient presented with acute LLQ pain.
US revealed an intact pregnancy of 8 weeks
and left of the uterus a painful, non-compressible (arrowheads), partly cystic,
partly solid mass, suspect for adnexal torsion.
At
laparoscopy a 360 degrees torsion of a luteal cyst was found.
After detorsion
the liquid component was aspirated.
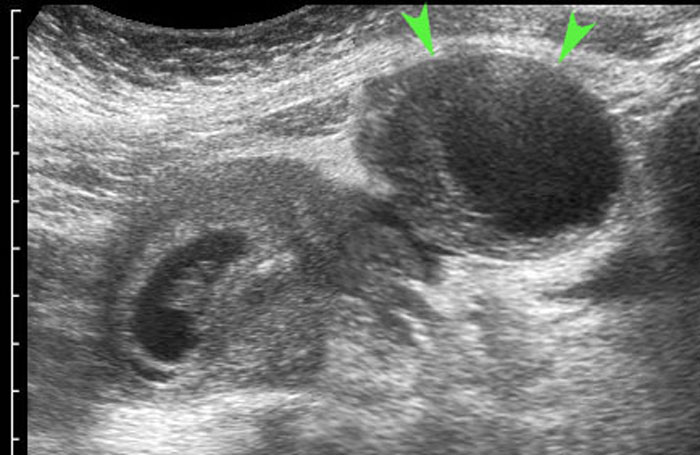
case 2
A 21-week pregnant woman was submitted with suspected appendicitis. She had similar attacks before.
US shows an intact pregnancy and in the right lower quadrant a large dermoid cyst (arrowheads).
At
laparotomy the dermoid cyst was oedematous, probably due to intermittent torsion.
Ovary-sparing resection was successful.
Acute conditions in non-Pregnant women
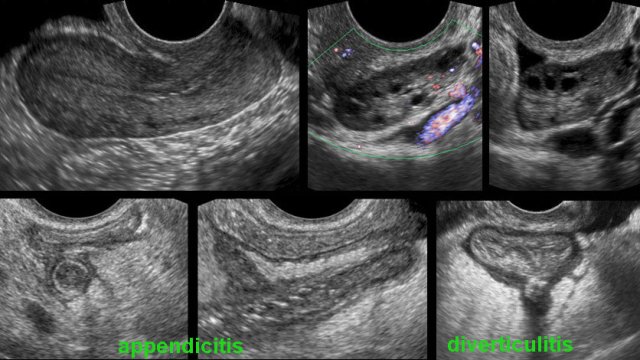
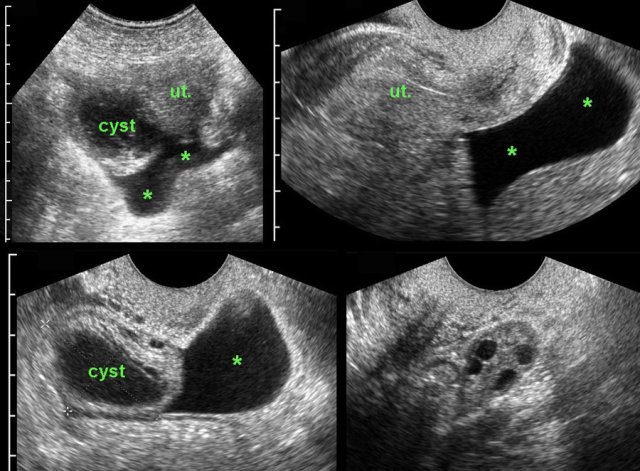
Persistent or hemorrhagic cyst.
In young
women with acute abdominal pain, an enlarged
cystic adnex with or without some free fluid, is a frequent finding.
In most cases, this is
a functional cyst, which has ruptured or has been bleeding.
Lab findings are
usually normal with a low CRP and the US
abnormalities disappear within days or weeks.
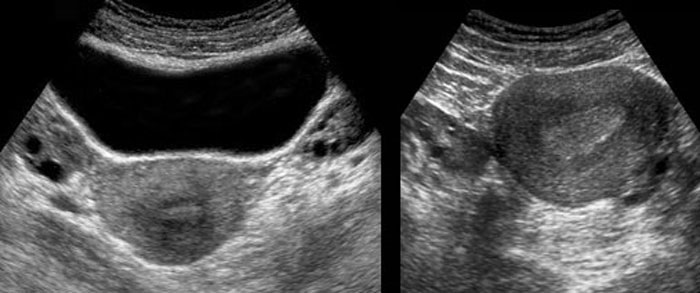
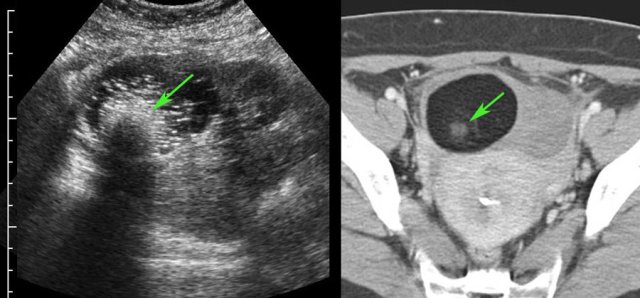
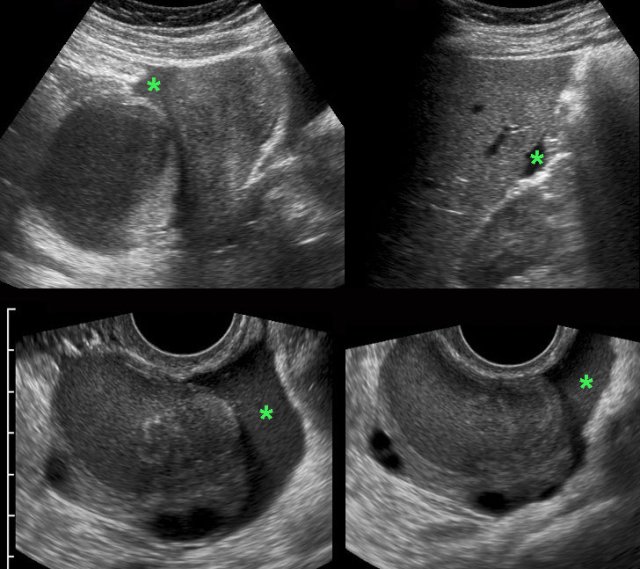
case 1
In this young woman a large partly cystic mass was found with a solid, avascular component (clot).
CRP remained low and the pain was gone in two days.
Follow up US after 6 weeks showed complete normalization.
It is important to realize that these US findings may also be completely asymptomatic.
case 2
In this young woman with two days of RLQ pain and a
CRP of 2, a right-sided, thin-walled ovarian cyst was found at US.
TVUS shows the typical, very thin, lace-like septations
and also the residual normal, follicle-containing ovary “squeezed” to the side
by the haemorrhagic cyst.
Complete resolution after 6 weeks.
case 3
These images are of a woman of 17 years old with acute, severe RLQ pain. CRP 1.
US reveals an ill-defined thick-walled right ovarian cyst and free fluid (*) in Douglas pouch.
TVUS confirms the fluid and a partially collapsed,
easily compressible cyst in the right ovary.
The left ovary is normal (right lower
image).
The pain gradually decreased and lab-findings remained normal.
Within one week there was complete
normalization of the US findings.
The most likely diagnosis: ruptured functional cyst.
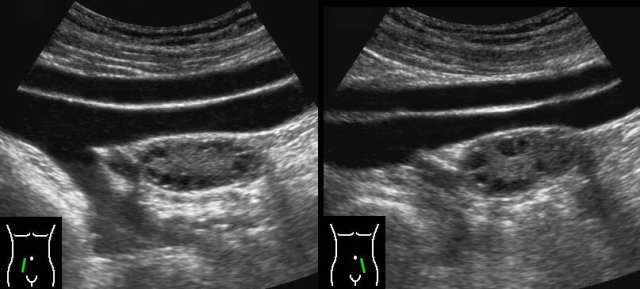
case 4
This functional, hemorrhagic cyst was a coincidental
finding and could easily be compressed against the promontory (p).
Complete resolution of the abnormalities within two weeks.
case 5
Persistent haemorrhagic cysts often contain solid,
avascular, inhomogeneous masses representing clots.
Retractility of such clots often results in concave contours (arrowheads).
case 6
In this young woman a conspicuous hemorrhagic right
ovarian cyst (arrowheads) was visualized and initially held responsible
for her RLQ symptoms.
Further examination however revealed an acute appendicitis
(arrow).
The cyst was an asymptomatic coincidental finding.
PID
Pelvic Inflammatory Disease (PID) is the common denominator for all ascending infections of cervix, endometrium, ovary and Fallopian tubes and its extension into the peritoneal cavity.
The causes are Chlamydia, gonorrhoea and Gram-negative organisms, but often cultures remain negative, and then the diagnosis is based on clinical findings and a good effect of antibiotics.
PID is often diagnosed and treated on clinical grounds, however US is often performed to diagnose and stage PID and to exclude alternative conditions as appendicitis.
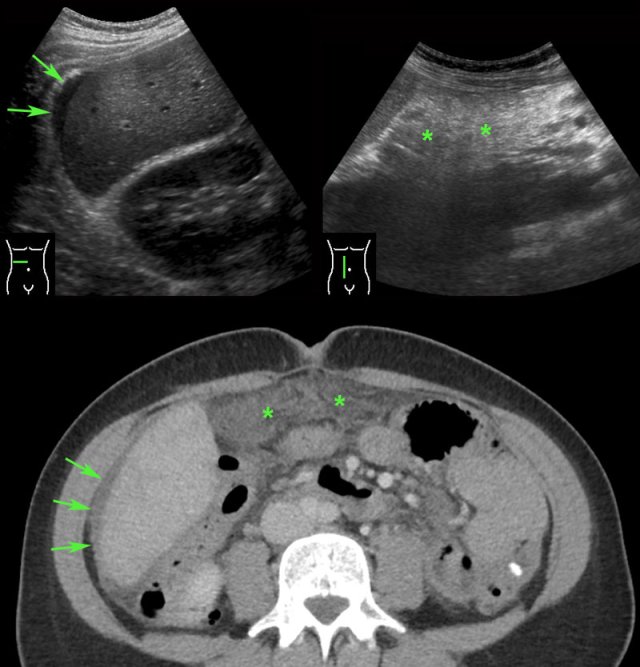
PID case 1
A 32 year old woman was treated for suspected cystitis with antibiotics by the family-doctor. Now submitted with clinically suspected appendicitis and CRP 190 and WBC 9.
US was normal, but of moderate quality due to obesity. CT showed an 8 mm, but otherwise normal looking appendix (arrow) and bilateral fatty stranding of the peritoneal fat (arrowheads).
The appendix looked “too normal” for a CRP of 190, so the most likely diagnosis was PID and antibiotics were started.
Two days later the PCR for Chlamydia was positive.
PID case 2
A young woman with severe pain in the LLQ and a CRP of 530 and a WBC of 22.
The only abnormal US finding was some hyperechoic preperitoneal
fat in the LLQ.
CT confirms the US findings.
Normal appendix and
adnexa (not shown here).
The most likely diagnosis was PID.
There was good reaction on antibiotics and no microorganism was found.
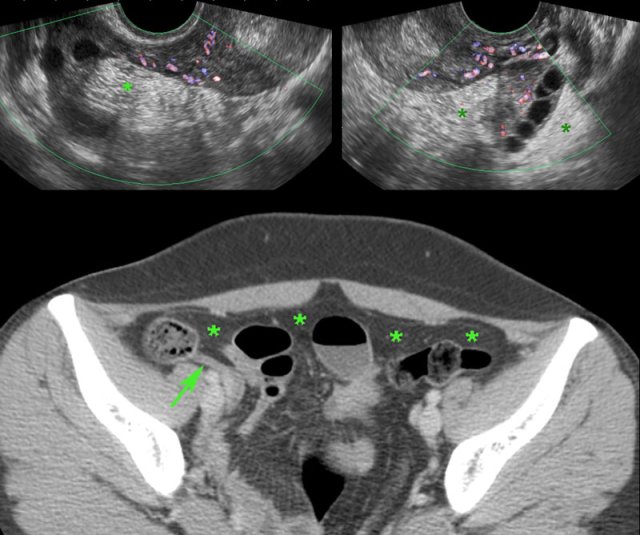
PID case 3
Young woman with acute RLQ pain and a CRP of 140.
Abdominal US was completely normal.
TVUS showed subtle hyperemia of both tubes and ovaries,
surrounded by hyperechoic, moderately compressible, fatty tissue (*).
This
represents slightly inflamed peritoneal, mesenterial and omental fatty tissue.
CT confirmed a normal appendix (arrows) and subtle diffuse hyperdensity of the peritoneal, mesenterial and omental fat (*).
She quickly recovered with antibiotics. Cultures and PCR remained negative.
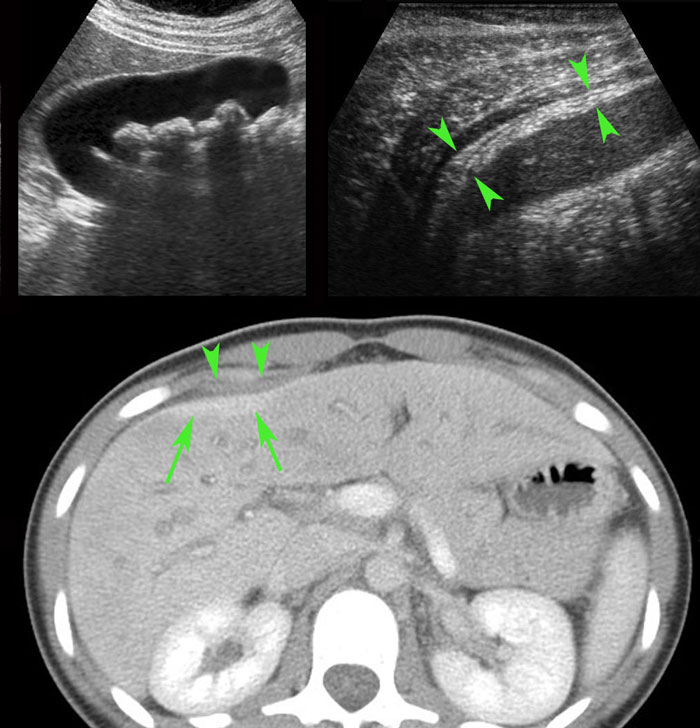
PID case 4
These images are of a very ill, painful young woman with generalized peritonitis and a CRP of 250, clinically suspect for perforated appendicitis.
US showed aperistaltic small bowel (b.).
The appendix
was not visualized.
TVUS showed a normal uterus and normal ovaries (arrowheads), which were surrounded by hyperechoic tissue (*).
CT confirmed the paralytic ileus and showed a normal appendix (arrow).
PCR was positive for gonorrhoea.
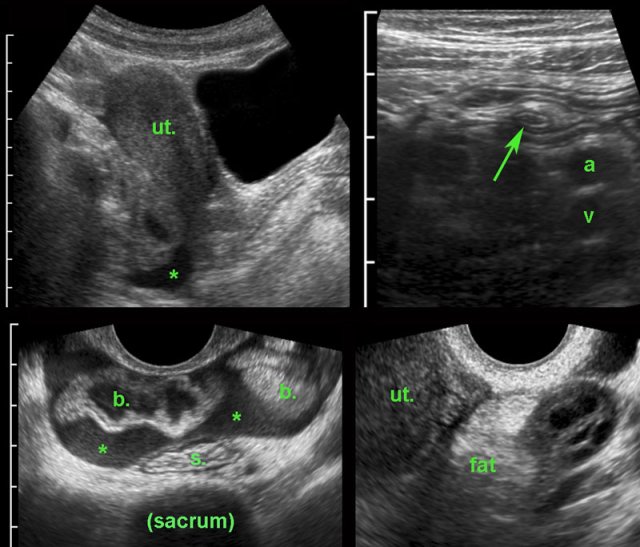 Early PID with secondary thickened appendix. (ut. = uterus, b = small bowel, a and v = iliac artery and vein, s = sigmoid)
Early PID with secondary thickened appendix. (ut. = uterus, b = small bowel, a and v = iliac artery and vein, s = sigmoid)
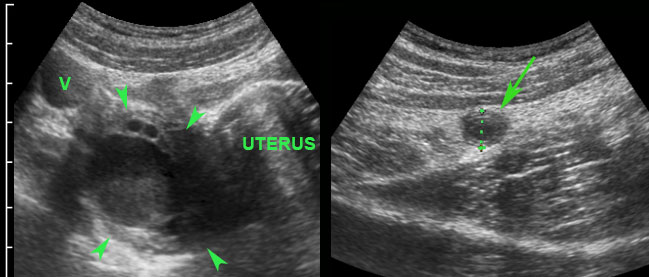
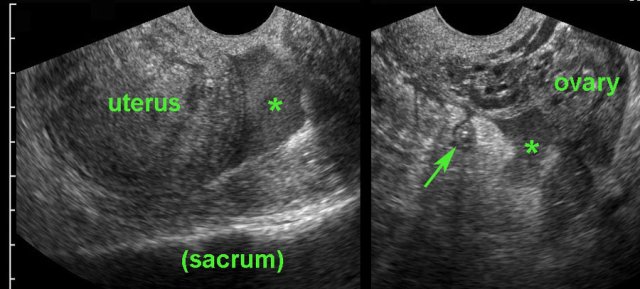
PID case 5
Young woman presented with RLQ pain and a CRP of 70, suspect for appendicitis.
US showed some turbid fluid in Douglas pouch (*).
At
the spot of maximum tenderness a compressible appendix (arrow) was seen, surrounded
by a little hyperechoic fat.
TVUS shows that the free fluid is turbid, in view of
the high CRP probably pus.
The ovaries had a normal aspect, but were surrounded
by hyperechoic, inflamed fat.
Diagnosis:
Early PID with minimal secondary reaction
of peritoneum and appendix.
One day later the PCR for Chlamydia was positive.
PID case 6
A 29-year old woman presented with suspected appendicitis. TVUS showed turbid fluid (*) in Douglas pouch, in combination with a CRP of 230, indicating pus.
The appendix (arrow) was small, but surrounded by hyperechoic fat. In view of the high CRP, it was decided that this was a case of PID with mild (secondary) inflammation of the appendix, rather than a case of appendicitis.
The patient was not operated, and responded well on antibiotics.
Key to avoid an unnecessary appendectomy in these
cases, is to note the discrepancy between the relatively mild inflammation of the
appendix and the high CRP.
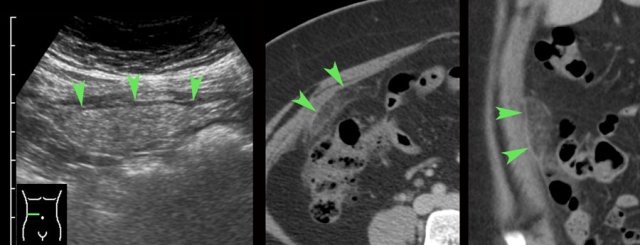
PID case 7
Ill young lady with suspected appendicitis, CRP 63, WBC
17.
The next day CRP was 400.
US showed a 8 mm appendix (arrows) and diffuse hyperechoic
fat in between hypoechoic tissue.
The ovaries were not well visualized.
CT confirmed a 9 mm appendix (arrows) and diffuse fat
stranding of the ventral fatty tissue (*).
Normal size and aspect of the ovaries
(not shown here).
At diagnostic laparoscopy a purulent peritonitis was
found and an abnormal appendix with fibrinous exudate was removed.
The pathological
specimen showed only peri-appendicitis, not primary appendicitis.
The day after the operation the PCR of the cervix was
positive for Chlamydia.
Omental infarction mimicking PID
A young woman presented with isolated pain in the RUQ and an elevated CRP.
The only abnormality at US and CT was a cake-like, rather outlined area of fat stranding adjacent to the ventral abdominal wall in the RUQ, just above the level of the umbilicus.
The shape and typical location strongly plead for segmental omental infarction rather than PID.
Familial Mediterranean Fever
A 27-year old woman had a history of two episodes of severe LLQ respectively RLQ pain, with a high CRP. She had no fever.
US was normal, but CT showed diffuse fatty preperitoneal
stranding (*).
Both times she was diagnosed with PID and treated with antibiotics.
Symptoms
disappeared, and cultures remained negative.
In view of her Turkish background, the third time the
diagnosis of Familial Mediterranean Fever was suggested, and eventually genetically proved.
She had no relatives
with FMF, but her parents were cousins.
No more attacks after colchicin.
Fitz-Hugh-Curtis
case 1
Young, ill lady with severe RUQ pain and an elevated CRP, clinically suspect for cholecystitis or perforated appendicitis.
US
shows a relatively high localization of an 8 mm appendix, which is well-compressible
(arrowheads), surrounded by some hyperechoic fat and clearly not responsible for
her clinical symptoms and lab findings.
Higher
up there is some free fluid and hyperechoic fat (arrows) around the tip of the
right liver lobe. No other abnormalities were found, especially normal aspect
of uterus and ovaries.
PCR
tests of cervix and urethra, one day later were positive for Chlamydia.
Diagnosis:
Fitz-Hugh-Curtis (FHC). FHC is also named “perihepatitis” and is in fact a sort
of “PID in the RUQ”, where the infection from the right Fallopian tube spreads directly
to the perihepatic space.
Late
sequelae of FHC are the well-known “violin string” adhesions between liver and
abdominal wall at laparoscopy.
case 2
A 29-year old woman presents with progressive pain in the RUQ during a week, radiating to her right shoulder. The family doctor determined her CRP, which was 145.
US
showed a little perihepatic fluid (arrows) and some fatty infiltration right of
the umbilicus (**).
CT confirms
the US findings. CA-125 was elevated (200). The differential diagnosis was FHC,
tuberculous peritonitis or malignant peritonitis. US guided omental biopsy
revealed no malignancy.
Two
days later PCR of cervix and urethra was positive for Chlamydia. Complete cure
after antibiotics.
case 3
Twenty year old woman with severe RUQ pain and a high CRP, suspect for acute cholecystitis.
US showed
a compressible, thin-walled gallbladder with multiple stones. This aspect is not
compatible with cholecystitis and does not explain the severe pain and the high
CRP. There was hyperechoic fat between the abdominal wall and the right liver
lobe (arrowheads).
CT
confirmed some perihepatic fat stranding (arrowheads) and (secondary) enhancement
of the subcapsular liver parenchyma (arrows), confirming the diagnosis of FHC.
One
day later the PCR was positive for Chlamydia.
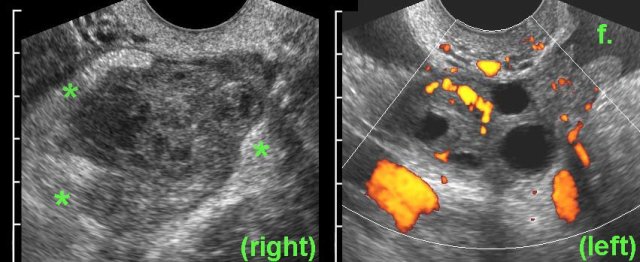
Oophoritis
case 1
Ill,
young woman with RLQ pain and a CRP of 160.
TVUS shows a hyperemic,
swollen right ovary, with irregularly defined, thick-walled follicles, filled
with debris-like material (pus), surrounded by hyperechoic fat (*).
PCR was positive for Chlamydia the next day.
case 2
Young woman with acute pain RLQ and a CRP of 75.
TVUS
shows an irregularly enlarged, inhomogeneous
right ovary with blurred follicles and surrounded by hyperechoic fat (*).
The left ovary is slightly hyperaemic, but otherwise
normal.
There is turbid fluid (f.) in Douglas pouch, representing pus (CRP 75).
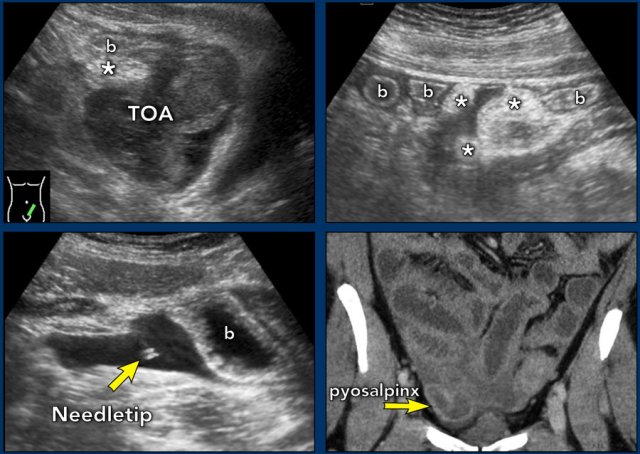
Tubo-ovarian abscess
TOA case 1
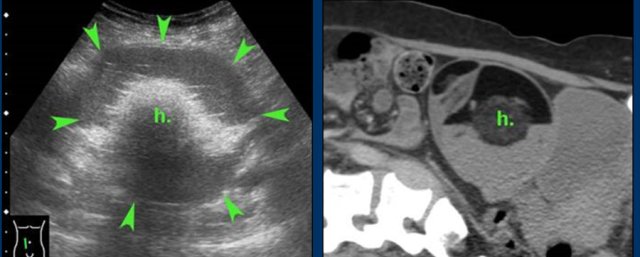
Young,
very ill woman with acute LLQ pain and a CRP of 260. Left of the uterus a massively
enlarged (6 x 7 x 8 cm) ovary is found.
The individual follicles are enlarged, ill-defined
and filled with turbid fluid (pus).
Note the hyperechoic halo around this inflamed
mass.
Since
there is no apparent involvement of the Fallopian tube, strictly speaking this
is an oophoritis.
Nevertheless, usually the term of tubo-ovarian abscess is used.
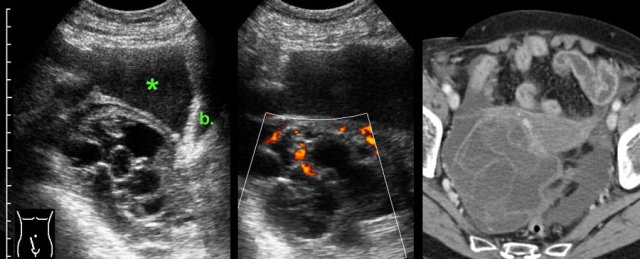
TOA case 2
Young
woman presenting with severe acute abdominal pain clinically suspect for perforated
appendicitis.
Lab-findings at admission: WBC 10.6 - CRP 6 Two days later: WBC 19.7 - CRP 459
US showed a large inhomogeneous masses left and
right of the uterus, suspect for tubo-ovarian abscess (TOA).
There
was also a paralytic ileus with secondary wall thickening of small bowel (b.) and
hyperechoic preperitoneal and mesenterial fat.
Puncture of a little ascites yielded
2 cc of yellow, turbid fluid.
CT
confirmed the US findings but additionally demonstrated a pyosalpinx (p.)
within the tubo-ovarian mass on the right side. Antibiotics are started intravenously.
Two
days later PCR of both cervical and urethral probes as well as the punctured
fluid were positive for Chlamydia.
Rapid recovery with only antibiotics.
TOA case 3
Large
left sided TOA with air-configurations.
This is a rare finding in TOA, successful
treatment with only antibiotics.
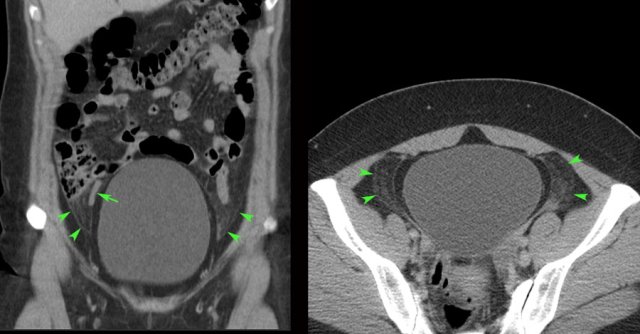
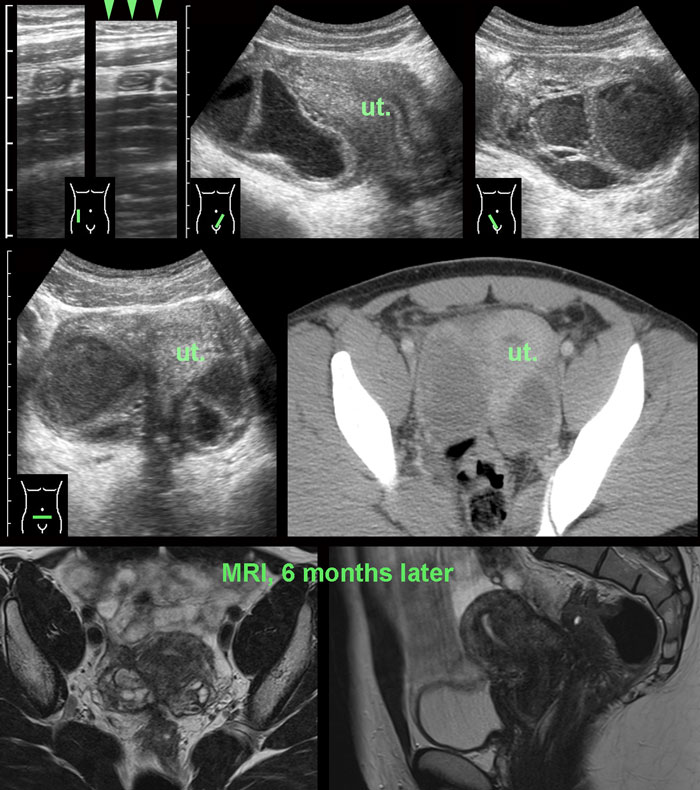
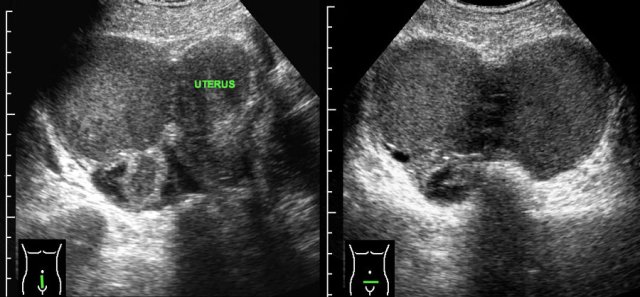
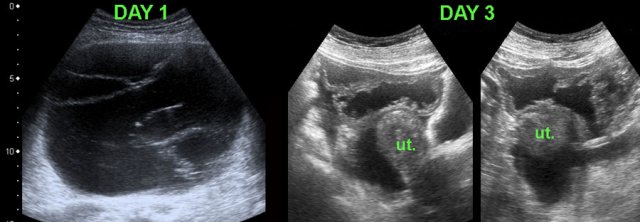
TOA case 4 (infected endometriotic cysts)
These images are of a 29-year old woman, suspected for appendicitis. CRP 185, WBC 17.
US shows a normal compressible appendix, thereby excluding appendicitis.
Large, thick-walled, septated cystic structures, filled with debris-like material, were found on both sides of the uterus (ut.), touching each other posteriorly (“kissing ovaries”).
This is somewhat suspect for bilateral infected endometrotic cysts.
The patient was treated with antibiotics and laparoscopic drainage.
There was a protracted course, but eventually regression of the abnormalities.
An MRI six months later, demonstrated all the signs of deep infiltrating endometriosis, also invading the rectum, thereby confirming the diagnosis of endometriosis.
case 5 - Actinomycosis
A 52-year old woman presented with RLQ pain for two weeks.
US and
subsequent CT, showed a large, right sided iliopsoas abscess (absc.), in continuity
with a TOA, causing hydronephrosis with cortical loss and a dilated ureter (u.).
There was an IUD in the uterus, the CRP was 240 and the WBC 26.
The
IUD, that had been in place for 30 years, was removed.
The abscess was punctured
and later drained percutaneously.
Gram
stain of the pus showed gram-positive rods, suggestive of actinomycosis, and
i.v. penicillin was started.
Cultures grew Actinomyces israelii 20 days later.
Eventually there was a complete cure without residual abnormalities.
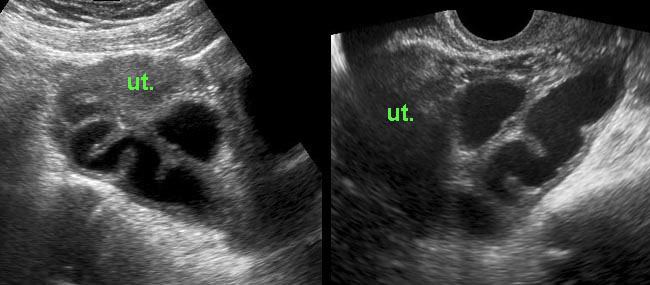
Pyosalpinx
case 1
these images are of a young woman with pain in the RLQ for two days and CRP 170 and WBC 14.
US respectively
TVUS shows tortuous, thick-walled tubular
structure right of the uterus (ut.), in combination with the CRP, typical for a
pus-filled Fallopian tube (pyosalpinx).
This
patient was successfully treated with antibiotics but had recurrent episodes.
For this reason she underwent
a tubectomy three years later.
case 2
Young lady with pain RLQ since three days. CRP 100 and WBC 23, suspect for appendicitis.
US shows
turbid peritoneal fluid and a dilated, thick-walled Fallopian tube, filled with debris. Complete cure after antibiotics.
case 3
Young woman with acute pain RLQ and a CRP 180, suspect for appendicitis.
US
confirms a IUD in the uterus and a large, right-sided pyosalpinx.
Complete
recovery after antibiotics and removal of the IUD.
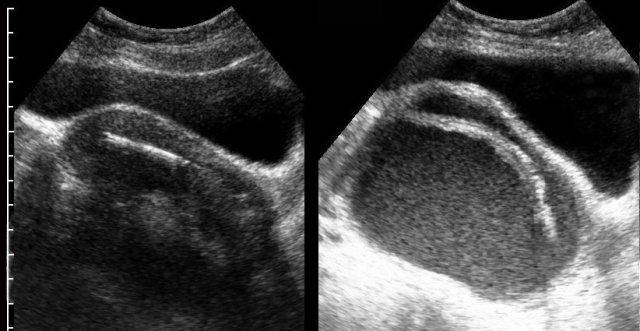
Torsion of enlarged adnex
case 1
Young female with acute onset of RLQ pain.
US
reveals a large mass filled with hypoechoic sebum, harbouring a hyperechoic hairball
(arrow) surrounded by multiple tiny linear
hair reflections.
CT confirms
a dermoid cyst containing a hairball
(arrow) and surrounded by fat stranding, caused by venous congestion.
At surgery
torsion of a dermoid cyst was confirmed.
case 2
A 40
year old lady presented with acute RLQ pain.
CT revealed a dilated, fluid-filled
salpinx.
Additional
US showed that the salpinx was under tense pressure and “bulged” into the
abdominal wall during compression (arrows).
An ischemic, twisted hydrosalpinx was found and laparoscopically removed.
case 3
In this 45-year old woman with acute lower abdominal pain, TVUS was negative.
Subsequent transabdominal US showed a large dermoid (arrowheads) in a fairly high location.
CT confirmed the diagnosis.
At surgery a twisted dermoid cyst was found.
Endometriosis
Endometriosis is endometrium outside the uterus.
There are three main types of endometriosis, based on where it is:
- Superficial peritoneal lesions. This is the most common kind. There are lesions on the peritoneum.
- Endometrioma or endometriotic cyst. These dark, fluid-filled cysts, also called chocolate cysts, form deep in the ovaries.
- Deeply infiltrating endometriosis. This type grows under the peritoneum and can involve organs like the rectum or bladder.
case 1
Young
woman with chronic lower abdominal pain and normal lab findings.
US demonstrates two large, thick walled ovarian cysts with homogeneous sludge-like (“chocolate”) contents behind the uterus.
The cysts are fixed to each other (“kissing
ovaries”) and to the uterus.
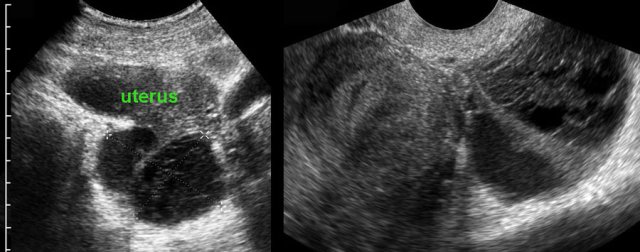
case 2
Patient with chronic lower abdominal pain and normal lab.
US
shows 5 cm, thick-walled cyst with triangular demarcation from the uterus,
indicating adhesions.
At
TVUS the cyst adhered completely to the uterus and during compression with the
vaginal probe, it was not possible to separate the cyst from the uterus.
Enlarged cystic adnex
In the
majority of women with acute abdominal pain and an enlarged, cystic adnex, the final diagnosis will be an ordinary haemorrhagic,
persistent or ruptured functional cyst.
There will be no other therapy than pain medication
and reassurance.
There are however several other pathological adnex-conditions that do have therapeutic consequences, and thus should be excluded like endometriotic cyst, dermoid cyst, a benign or malignant tumor, hydrosalpinx or a tubo-ovarian abscess (see Table).
Next to clinical features and lab findings, US has an important role to differentiate these conditions from a functional cyst.
Therefore in case of relatively mild
symptoms and conservative treatment, a cystic adnex is generally followed up by
US after six weeks.
If completely disappeared by then, it must have been a
case of a hemorrhagic, persistent or ruptured functional cyst.
case 3
Young female with peracute pain in the lower abdomen since 4 hours. WBC 20, CRP 17.
US
shows large, thick-walled, partly cystic mass right of the uterus and some turbid free
fluid (*).
TVUS
shows that the endometriotic cyst is filled with homogeneous, hyperechoic fluid
(old blood) and is easily compressible (as expected after rupture).
Ruptured cystadenoma.
case 1
An elderly lady presented with peracute RLQ pain and leucocytosis.
US
and subsequent CT showed a collapsed, multicystic tumour with thick-walled,
hypervascular septa and free fluid (*).
The bladder (b.) was empty.
Surgery
revealed a ruptured cystadenoma, which was benign at histology.
case 2
These images are of a woman of 56 yrs with diffuse abdominal pain and bloating.
US revealed a very large cystic,
septated mass of 15 x 18 x 20 cm.
There was no ascites. She was planned for
laparotomy within one week.
Three
days later she presented at the hospital with acute pain.
US showed a collapsed
cyst with massive intra-peritoneal fluid.
At laparotomy a ruptured, benign, mucinous
cystadenoma was removed.
Twelve years later she is still doing fine.
case 3
This young
woman presented with acute lower abdominal pain.
US
showed a right sided hyperechoic mass and a lot of free fluid (not shown here). CT
confirmed a small dermoid cyst and hyperdense ascites, probably blood.
Operation
revealed a ruptured dermoid cyst, the free fluid is a mixture of blood and
sebum.
Post Partum
Ovarian vein thrombosis
case 1
Four days after delivery this young woman developed
pain in the RLQ and a CRP of 125.
At the spot of maximum pain an ill-defined, solid,
tubular, hypoechoic structure (*) was seen, surrounded by hyperechoic, non-compressible,
inflamed fat (arrowheads).
CT confirmed an ovarian vein thrombosis. The surrounding
fat-stranding suggested a concomitant, phlebitis-component.
Complete recovery with antibiotics and anticoagulant therapy.
case 2
This patient presented with RLQ pain 5 days after the procedure.
US demonstrated a thrombus in the right ovarian vein, there was no clear phlebitis
component.
CT confirmed a thrombus in the right ovarian vein, without
any fat stranding.
CRP remained low.
Complete cure with only anticoagulant therapy.
Epilogue
The author thanks his fellow radiologists and gynaecologists for their valuable help in collecting all the educational material.
A special thanks to gynaecologist Jan Lind, for his advice in editing the manuscript.
Charity
All the profits of the Radiology Assistant go to Medical Action Myanmar which is run by Dr. Nini Tun and Dr. Frank Smithuis sr, who is a professor at Oxford university and happens to be the brother of Robin Smithuis.
Click here or on the image below to watch the video of Medical Action Myanmar and if you like the Radiology Assistant, please support Medical Action Myanmar with a small gift.

torsio-dermoid-gravida-coll-1-pijlen.jpg/bfd8c0c809cda57b553f9ef1da388950/15-)torsio-dermoid-gravida-coll-1-pijlen.jpg)

funct-cyste-zeker-coll.jpg)

gonorr-pid-ov-ut-gb-paral-ileus-coll-2.jpg/a7d94aba0563c0db023a7f24b3844f66/27-)gonorr-pid-ov-ut-gb-paral-ileus-coll-2.jpg)

-coll.jpg/22339d725813e3f5104cd845d647f6ef/25-toen-diagn-pid-(bleek-fmf)-coll.jpg)
fitz-hugh-curtis-coll2.jpg/355e8a09daed4df40bb3142d57bc3440/31-)fitz-hugh-curtis-coll2.jpg)
pid-coll.jpg/44d80986fc45369eced905f3ace3cba7/34-)pid-coll.jpg)
toa-ecoli-ziek-coll-eng.jpg/e2f13b033254bbb5c0795c8d6f054d0b/36-)toa-ecoli-ziek-coll-eng.jpg)

-pyosalpinx-coll.jpg)
ovthromboseleekapp-coll.jpg/c4dc923192c25ce0cd38721399b1dba5/51-)ovthromboseleekapp-coll.jpg)