CT and MRI of the Eye
by David Yousem
Neuroradiology department of the Johns Hopkins Hospital in Baltimore
Publicationdate
This review is based on a presentation given by David Yousem and adapted for the Radiology Assistant by Robin Smithuis.
David Yousem is currently the Director of Neuroradiology and Professor of Radiology at the Johns Hopkins Hospital.
He is also the editor of the book 'Neuroradiology: the Requisites'.
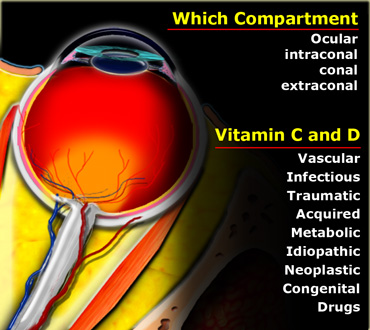
In this article a systematic approach to orbital pathology is presented based on division of the orbit into the following compartments:
- Ocular space
- Intraconal space
- Conal space
- Extraconal space
Anatomic Considerations
The first thing you do when you see a lesion in the orbit, is to decide whether it is an ocular lesion or a non-ocular lesion, i.e. is it involving the globe or involving the structures outside the globe.
If it is a non-ocular lesion, the next question is whether the lesion is located within the intraconal space, i.e. within the space bounded by the cone formed by the extraocular muscles, or whether it is located within the conal or extraconal space?
Once you have decided where the lesion is located, consider the differential diagnostic possibilities using the mnemonic VITAMIN C and D.
We will first describe the anatomic spaces of the orbit and summarize the pathology within these spaces, even if some of these pathologies are not visible radiologically.
Then we will discuss the radiological findings in certain orbital diseases.
Ocular space
The eye has the following well defined anatomic spaces:
Anterior chamber
When we move from anterior to posterior the first area is the anterior chamber.
It is bounded by the cornea anteriorly and the lens and iris posteriorly.
Specific pathologies within the anterior chamber are:
- Rupture of the globe
- Hemorrhage: also known as anterior hyphema
- Cataract
- Keratitis: inflammation of the cornea
- Periorbital cellulitis
Posterior chamber
This is a very small area posterior to the iris, which we cannot discern on imaging.
Specific pathologies in this area are: glaucoma, uveitis and ciliary melanoma.
Vitreous body
The larger area posterior to the lens is the vitreous body.
Specific pathologies within the vitreous body are:
- Rupture
- Hemorrhage
- CMV infection: especially in HIV
- Persistent Hyperplastic Primary Vitreous (PHPV): primary vitreous failed to develop into secondary clear vitreous leading to blurred vision
- Reinflation procedures for detachments leading to different densities within the vitreous body
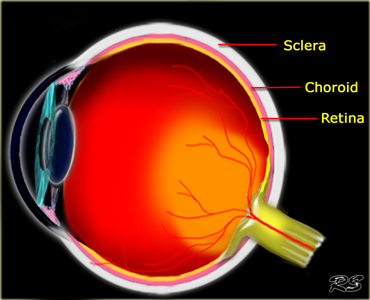
The vitreous body is surrounded by the membranes of the retina, the choroid and the sclera.
Retina pathology:
- Retinoblastoma: a common tumor in children
- Hemangioblastoma: most common retinal tumor in the adult and associated with von Hippel Lindau disease
- Detachment: most common retinal lesion mostly seen in diabetic retinopathy
Choroid pathology:
- Melanoma: choroid contains the melanin cells
- Metastases: choroid is the most vascular structure in the eye
- Detachment: usually post-traumatic
Sclera pathology:
- Infection: either due to sinusitis or viral
- Pseudotumor
- Detachment
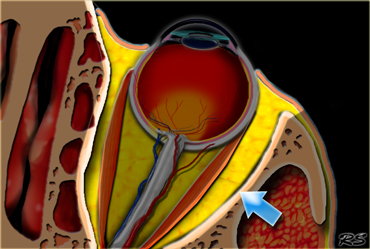
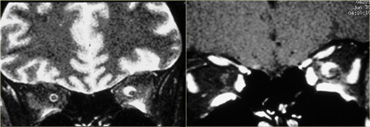
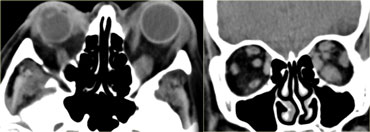
 The intraconal space is marked by arrows and is located within the muscle cone It contains the optic nerve, vessels and cranial nerves III, IV and VI.
The intraconal space is marked by arrows and is located within the muscle cone It contains the optic nerve, vessels and cranial nerves III, IV and VI.
Intraconal space
The ocular muscles within the orbit form a muscle-cone.
These ocular muscles are connected via the annulus of Zin, which is a fibrous connective tissue sheet and together they form the conal space.
It separates the intraconal from the extraconal space.
Intra-orbital pathology which is non-ocular is either in the intraconal, conal or extraconal space.
Intraconal space pathology:
- Venous vascular malformation
- Capillary hemangioma
-
Optic nerve lesions
-
Optic neuritis
- MS
- Devic's syndrome
- Neuritis due to infection (e.g.herpes zoster)
- Autoimmune (e.g.Lupus)
- Drugs (e.g.chloramphenicol, ethambutol)
- Optic nerve glioma
- Optic nerve meningioma
- Pseudotumor
-
Optic neuritis
-
Venous dilatation
- Carotid Cavernous Fistula
- Varices
- Schwannoma of 3rd, 4th and 6th cranial nerve
Conal space
The conal space is formed by the ocular muscles and an envelope of fascia.
Conal space pathology:
- Thyroid eye disease; usually enlargement of the inferior and medial rectus
- Pseudotumor: idiopathic orbital inflammation
- Adjacent inflammation: sinusitis
- Uncommon causes of enlargement of the extra-ocular muscles are glycogen storage disease and lymphoma.
Extraconal space
The extraconal space is the area outside the muscle cone.
Extraconal space pathology:
- Abscess due to sinusitis
- Schwannoma of the V1 and V2 branches of the trigeminal nerve
-
Bone lesions:
- Fibrous dysplasia of the sphenoid wing
- Metastases
- Multiple myeloma
- Diseases of the orbital appendages
Orbital appendages
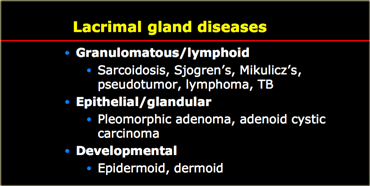
The lacrimal gland is located superolaterally in the orbit.
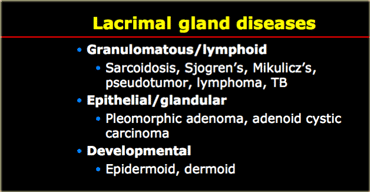
Diseases of the lacrimal gland can be divided into granulomatous, glandular and developmental (see Table).
Secretions go medially across the globe and are collected in the punctum and then go into the lacrimal sac.
From the lacrimal sac secretions travel inferiorly to the nasal lacrimal duct, which drains under the inferior terminate into the nose.
In children congenital obstructions of the valves in the lacrimal duct can lead to cystic areas medially in the orbit also known as dacryocystoceles.
In adults obstruction is more often due to strictures from ethmoid sinusitis or stones blocking the nasolacrimal duct.
This will result in epiphera or increased tearing.
Drainage can be improved with balloon dilatation.
Ocular pathology
Calcifications
In adults the most common intraorbital calcifications occur at the tendinous insertion of the ocular muscles.
Other common calcifications are at the optic nerve head within the eye, also called 'optic disc drusen'.
These are usually asymptomatic, but when the ophtomologist inspects the eye, there is the impression of papilledema, i.e. pseudo-papilledema.
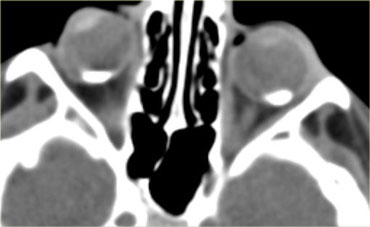
In children calcifications in the globe means retinoblastoma until proven otherwise even if it is bilateral.
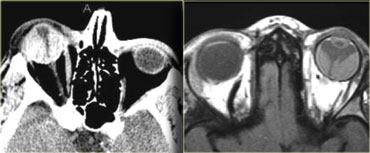
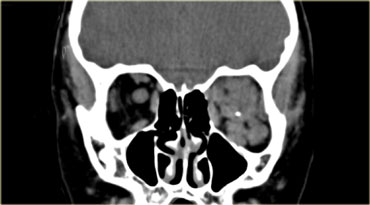
On the left an image of an adolescent with bilateral retinoblastoma.
Retinoblastoma
As you can see in the table on the left, retinoblastoma is a one of the more common tumor in the first year of life.
The other tumors in this age group are neuroblastoma, Wilm's tumor, leukemia and teratoma.
All bilateral cases are hereditary and result from a deficient tumor suppression gene on chromosome 13.
The diseases that are listed in the differential diagnosis are all uncommon.
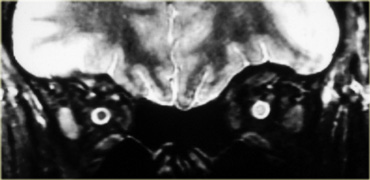
On the left images are of a 13 month old female with bilateral lesions as a result of bilateral retinoblastoma.
Small retinoblastomas are treated with different kinds of therapy (cryoablation, laser photocoagulation, chemothermotherapy, brachytherapy, plaque radiotherapy) in order to save the eye and avoid enucleation.
If the patent is treated with radiation, there is a 30% chance of a second malignancy within the radiation field, due to the radiation but also due to the deficient tumor suppression gene.
Outside the radiation field there is an 8% chance of malignancy.
In order of frequency: Osteosarcoma > other sarcoma > melanoma > carcinoma.
These patients are also at risk for pineal tumors and parasellar PNETs.
The pineal gland is considered as the third eye and the third testicle.
Meaning, you can develop retinoblastoma in the pineal gland, i.e. trilateral retinoblastoma, but also germinoma.
Always examine the brain in these patients and remember that at the age of 0-4 years, which is the peak age for retinoblastoma, the pineal gland does not calcify, so any calcification in this region is suspicious of retinoblastoma.
On the left images are of another patient with retinoblastoma.
This tumor presents as a large calcification.
When a retinoblastoma occupies more than half of the globe, as in this case, the eye has to be enucleated.
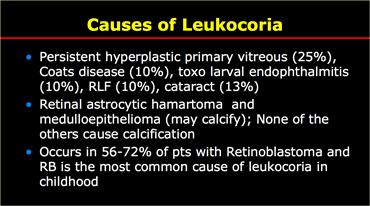
Leukocoria
Usually, when a light shines through the iris, the retina appears red to the observer.
In leukocoria (white pupil) the retina abnormally appears white.
Retinablastoma is usually detected through leukocoria as it occurs in two third of patients with retinoblastoma.
These children are usually too young to present with visual complaints.
There are many causes of leukocoria as listed in the table on the left.
Melanoma
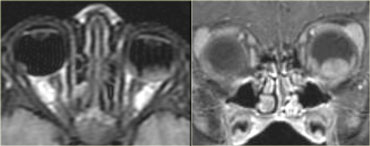
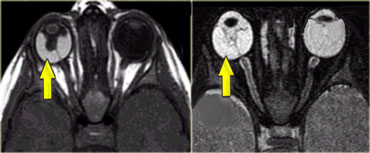
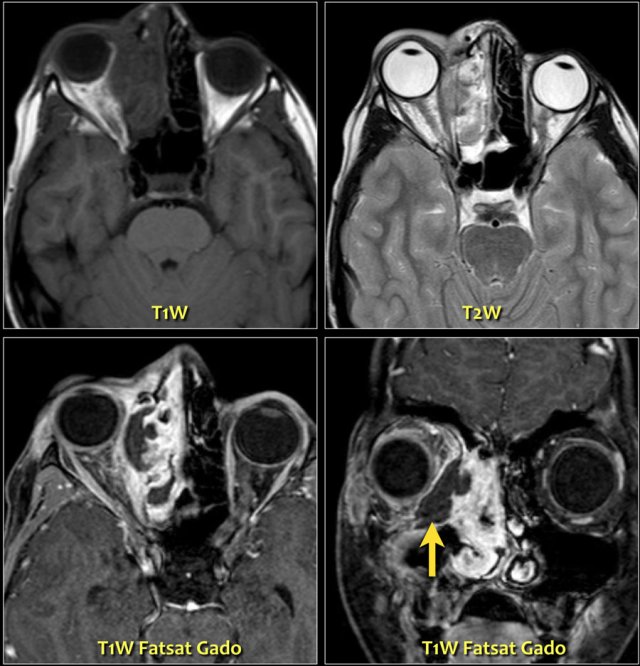
On the left images of an adult with an ocular mass.
The most common intraocular lesion in an adult is melanoma (as in this case).
Number two is metastases and others like hemangioma, leiomyoma and osteoma are uncommon.
Persistent hyperplastic primary vitrous (PHPV)
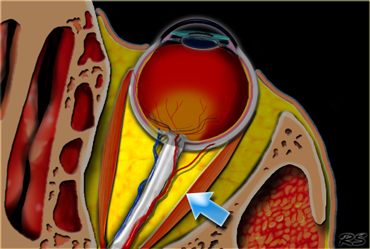
On the left another cause of leukocoria.
This is persistent hyperplastic primary vitrous (PHPV).
There is a persistent hyaloid canal when the hyaloid artery does not integrate.
On the images we see a persistent canal that goes from the optic nerve to the lens.
There is also retinal detachment (occurs in 30-55%) and notice the microphtalmia.
PHPV is the second most common cause of leukocoria.
These patients also develop glaucoma and cataract.
Coats' disease
Coats' disease is a rare eye disorder of unknown cause, leading to full or partial blindness, characterized by abnormal development of blood vessels behind the retina.
Globe rupture
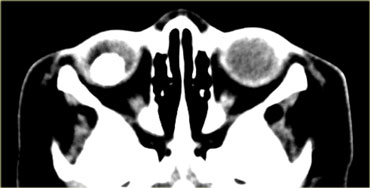
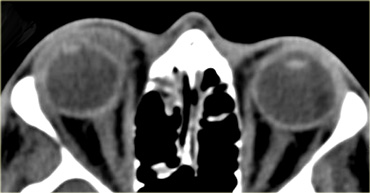
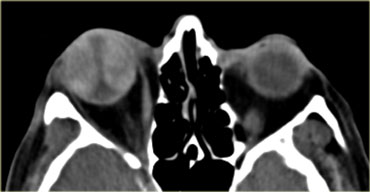
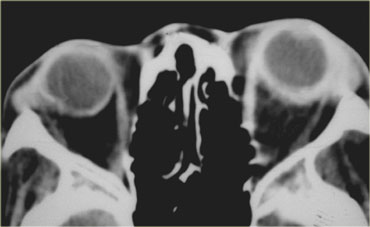
On the left images of a patient who presented in the ER with post-traumatic orbital swelling.
This patient has globe rupture and specifically rupture of the anterior chamber.
As radiologists we are used to looking at the vitreous body if we think of globe rupture, but that is not enough.
Notice that the depth of the anterior chamber is decreased.
There is increased density anteriorly as a result of hyphema (blood in the anterior chamber).
Also notice that the lens on the right side is blurred and slightly less dense.
This is called a traumatic cataract.
Maybe you would have expected the lens to be more dense, but that is usually not the case.
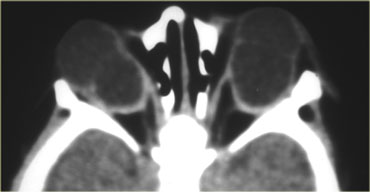
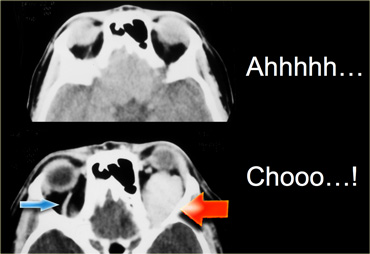
On the left CT images of a patient who had a left eye trauma.
Study the images for 5 findings and then continue reading.
The findings are :
- The anterior chamber is shallow compared to the right side indicating globe rupture.
- The density in the anterior chamber is higher indicating hyphema.
- The density of the lens is lower, so this patient has a traumatic cataract.
- There is an area of high density in the vitreous body indicating hemorrhage.
- The globe is flat on the posterior side so there is vitreous rupture as well.
Globe rupture is seen most commonly at the anterior chamber.
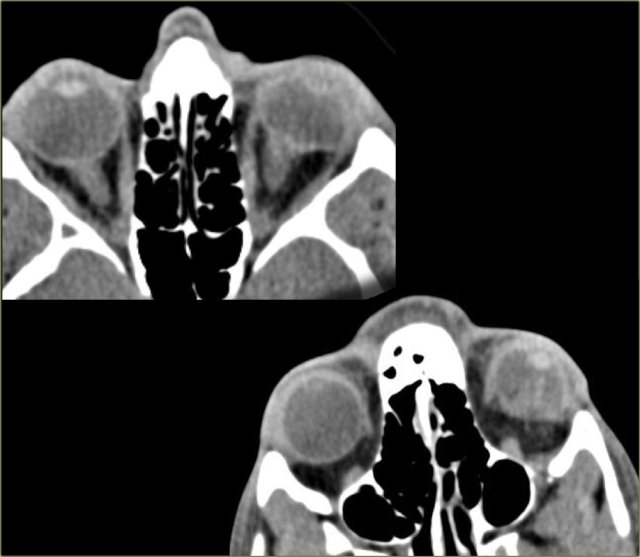
Retinal and choroidal detachment
Blood can be located in the following locations:
- Anterior chamber: anterior hyphema
- Posterior chamber: posterior hyphema (too small to see)
- Vitreous: vitreous hemorrhage
- Choroidal detachment
- Retinal detachment
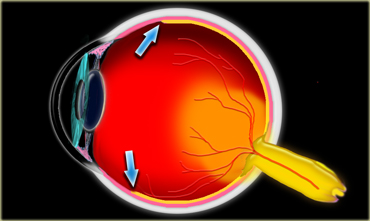
Retinal detachment can be distinguished from choroidal detachment, because the retinal epithelium ends at the ora serrata (figure).
Evidently a retinal detachment will not go beneath this point.
Retinal detachment with haemorrhage is seen mostly in adults with diabetes mellitus and hypertension.
In young infants it can be seen as part of a shaken baby syndrome.
In choroidal detachment recent intraocular surgery is the most common association followed by trauma.
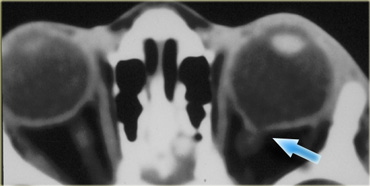
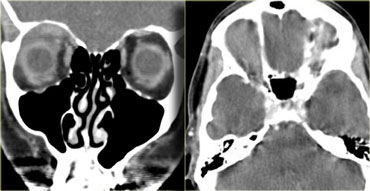
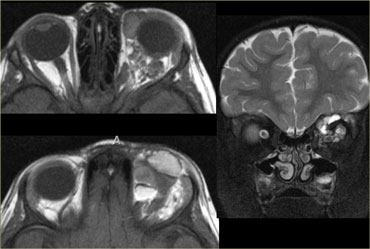
On the far left a CT of a choroidal detachment going beyond ten and two o'clock (with the lens at twlve o'clock) and evidently more anteriorly to the ora serrata.
It looks as if the detachment ends at the optic nerve but, if you look carefully, the choroidal detachment actually crosses the optic nerve.
That would be very unusual for a retinal detachment, but is sometimes seen in choroidal detachment.
On the right a T1WI of a retinal detachment.
It ends at the optic nerve and at the ora serrata.
On the left an image of another case of choroidal detachment.
Coloboma
Coloboma is a congenital malformation in which part of the eye does not form due to failure of fusion of an embryonic structure called the intraocular fissure.
Often there is microphtalmia and the eye protrudes inferiorly.
In 10% there are other CNS anomalies.
On the left images of a patient with bilateral colobomas.
Coloboma can be part of the CHARGE syndrome:
- Coloboma
- Heart anomalies
- choanal Atresia
- Retardation of growth and development
- Genital and Ear anomalies.
Coloboma can also be part of the COACH syndrome:
- Cerebellar vermis hypoplasia,
- Oligophrenia (MR)
- congenital Ataxia
- Coloboma
- Hepatic fibrosis.
On the left images of a patient with a small coloboma at the entrance of the optic nerve.
The patient on the left had a coloboma and also agenesis of the corpus callosum with an associated midline lipoma.
Intraconal pathology
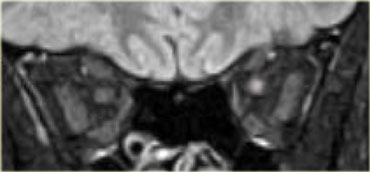
Devic's syndrome
Devic's syndrome is also known neuromyelitis optica.
Let's first look at the images and then discuss it in more detail.
On the left image there is a normal optic nerve on the right side.
Notice that the optic nerve is white matter tract.
It has the same signal intensity as the white matter in the brain.
On the contralateral side there is high signal intensity in the optic nerve.
This is therefore extra-ocular intraconal disease and we will be thinking of neoplastic versus demyelinating diseases.
Continue with the next image.
On the left a FLAIR image with fat-sat.
Notice the abnormal signal intensity and the fact that the optic nerve is not enlarged, which argues against the possibility of a tumor.
Images of the cervical spinal cord show a long segment of non-space occupying disease.
Based on these images the differential diagnosis is MS and Devic's syndrome (also caled neuromyelitis optica).
Since MS is far more common, this would be the most likely diagnosis, but this happened to be Devic's syndrome.
Some consider Devic's syndrome as a form of MS, but Devic's syndrome differs from MS:
- The patients are very ill, as Devic's is more acute and more fulminant.
- Usually there is a combination of one-sided blindness and paraparalysis due to the long segment of transverse myelitis (in MS it is usually one- or two-segment).
- Devic's is usually monophasic.
- Usually no brain plaques.
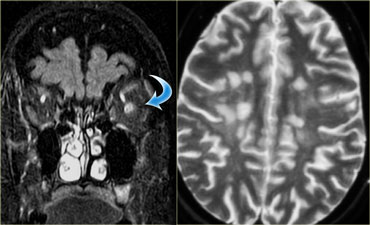
MS
On the left images of a different patient, who also has optic neuritis.
There is high signal in the optic nerve and in the brain there are multiple lesions as a result of MS.
These lesions did not occur at the same time, so there is dissemination in time and in place, which is specific for MS.
-
50% of patients with optic neuritis eventually develop MS.
The other 50% have isolated optic neuritis (see differential diagnosis above). - 80% of patients with MS develop optic neuritis at some point in time.
Meningioma
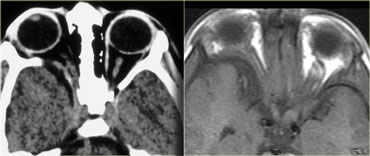
On the left images of another patient with extra-ocular intraconal disease.
First look at the images, describe them and come up with a differential diagnosis (for a moment disregard the fact that the title of this paragraph is meningioma).
The optic nerves are normal, but there is abnormal mass-like enhancement of the optic nerve sheath on the left.
So this is probably a neoplasm and of the neoplasms meningioma is by far the most common optic nerve sheath tumor.
Meningiomas present with visual disturbances early in the course of the disease as a result of ischemic neuropathy due to venous obstruction.
Clinically this presents as a pale disk.
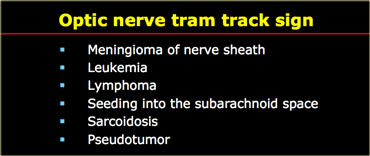
Abnormal enhancement of the optic nerve sheath
On the left a table with the differential diagnosis of abnormal enhancement of the optic nerve sheath, also called
optic nerve tram track sign.
Meningioma of nerve sheath is a result of subdural growth leading to progressive visual loss, papilledema, optic atrophy.
There is a strong association with NF-2.
The pale disk is due to venous outflow impairment.
Calcifications are seen in 20-50%.
Seeding into the subarachnoid space is another cause of abnormal ennhancement of the optic sheath due to the fact, that the sheet of the optic nerve communicates with the intracranial compartment of the subarachnoid space).
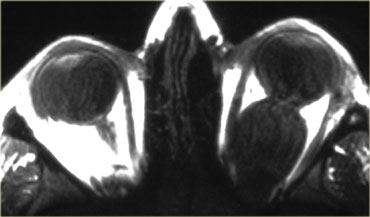
Optic nerve glioma
First look at the images on the left.
Which side is abnormal and what is the most likely diagnosis?
There is sphenoid wing hypoplasia on the right and on the left the optic nerve near the chiasma is enlarged (visible on the MR).
So the diagnosis is neurofibromatosis type I with sphenoid wing hypoplasia and an optic pathway glioma.
The term optic nerve glioma is a misnomer.
Actually the tumor can present anywhere along the optic tract from the occipital region to the chiasm and the optic nerve.
The term glioma is also rather non-specific.
These tumors are juvenile pilocytic astrocytomas WHO type 1, which is the most benign form of astrocytoma.
They make up 4% of all orbital tumors.
More than 50% of patients who have an optic nerve glioma have NF1, but in NF1 only about 10% have optic nerve glioma.
They are less commonly cystic in NF than in non-NF.
The mean age at diagnosis is 4-5 years and only 20% of these patients have visual symptoms, because the glioma does not affect the optic nerve early and because these small children do not complain of vision problems.
On the left another case with a more typical example of optic nerve glioma also in a patient with NF1.
 LEFT: multiple iris hamartomas (Lisch nodules) RIGHT: axillary freckling (small brown spots) and caf? au lait spots
LEFT: multiple iris hamartomas (Lisch nodules) RIGHT: axillary freckling (small brown spots) and caf? au lait spots
The criteria for the diagnosis of NF1 are met in an individual if 2 or more of the following signs are found:
- Six or more caf? au lait macules
- Two or more neurofibromas of any type or 1 plexiform neurofibroma
- Multiple freckles in the axillary or inguinal region
- Bone dysplasias
- Optic glioma
- Two or more iris hamartomas (Lisch nodules)
- A first-degree relative with NF1
Conal pathology
Thyroid eye disease
Take a look at the images on the left, describe them and come up with a differential diagnosis and again disregard the title of this paragraph.
The diagnosis is thyroid eye disease and the differential diagnosis is pseudotumor of the orbit.
In a moment we will discuss how to differentiate these two diseases.
In the past the term Grave's ophtalmopathy was used.
This however suggested that the patient is hyperthyroid.
Nowadays we know that patients that are treated for Graves disease can be euthyroid or even hypothyroid and still develop thyroid eye disease and therefore nowadays we use the term thyroid eye disease.
The great danger of thyroid eye disease is compressive optic neuropathy either due to direct compression by the muscles or ischemic by compression of the vessels.
The key feature to look for is the orbital apex.
If you do not see any fat around the orbital apex, there is a great chance of compression.
These patients are treated with decompression through an endoscopic procedure in which the medial wall of the orbit i.e. the lamina papyracea is crushed.
Pseudotumor
Take a look at the images on the left.
This is a case of pseudotumor.
Pseudotumor is idiopathic inflammation of the orbit.
It can affect every part of the orbit: muscles, tendons, fat, optic nerve, nerve sheet, lacrimal gland etc.
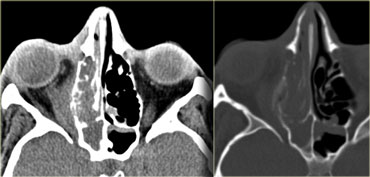
The key distinction between pseudotumor and thyroid eye disease is the fact that in pseudotumor not only the muscles, but also the tendons are involved.
These patients feel pain when they are moving their eyes as the tendons get irritated.
On the image on the far left notice the tapering of the swollen muscle at the point of the tendinous insertion in a patient with thyroid eye disease.
Next to it the images of the patient with pseudotumor.
Notice that the swelling includes to the tendinus insertion.
Extraconal pathology
Periorbital abscess
On the left nonenhanced CT-images of a patient with a evident periosteal or periorbital abscess as a result of a complicated ethmoid sinusitis.
The teaching point to make is the following:
Do not wait for peripheral enhancement to call it an abscess!
In every other location you wait for nice rim enhancement to call it an abscess and if not you say it is a phlegmone.
The treatment is the treatment of the sinusitis.
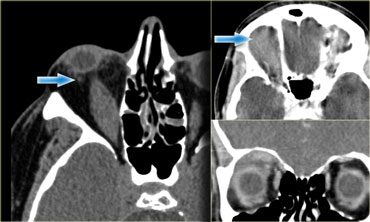
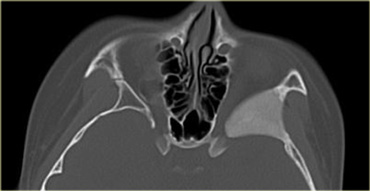
Here MR-images of an eleven year old boy, who experienced some irritation of his right eye the night before and woke up with a proptosis.
The enhanced T1W-images with fatsat nicely demonstrate a periorbital abscess which causes the proptosis.
Notice the ethmoid sinusitis.
The other teaching point to make is the following:
In children be very careful about extension outside the sinuses!
Any change outside the sinus should be called an abscess.
In children the periorbita is far more fenestrated and disease will easily spread.
So be aggressive in calling small abnormalities an abscess.
Periorbital abscess can lead to venous thrombosis of the superior and inferior ophtalmic vein.
In certain fungal sinusitis (e.g.aspergillosis) you can even get cavernous sinus thrombosis and cavernous-carotid fistula
Orbital and periorbital cellulitis
On the left images of a patient who presented in the ER with a 'red hot eye' and proptosis.
Now the difference between orbital and periorbital cellulitis is an important one and is based on an anatomic structure, which is called the orbital septum.
If a patient comes in the ER with a red hot eye and the inflammation includes the orbital septum and everything superficial to it, the diagnosis is periorbital cellulitis and the patient is treated with oral antibiotics on an outpatient basis.
In the case on the left however the structures posterior to the septum are also involved.
This patient has an orbital cellulitis and will have to stay in the hospital to receive antibiotics intravenously.
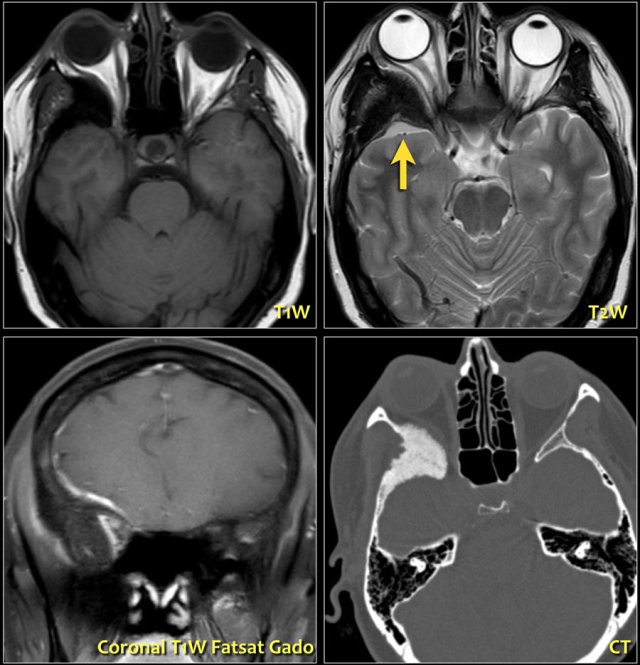
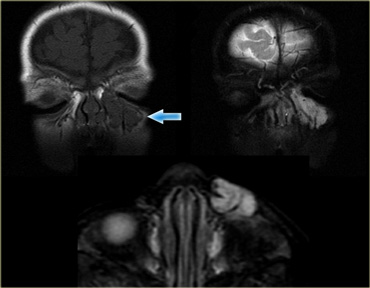
Sphenoid wing lesions
On the left a CT image of a patient with proptosis due to a sphenoid wing lesion.
There are four sphenoid wing lesions that can cause proptosis:
- Sphenoid wing dysplasia
- Fibrous dysplasia
- Paget's disease
- Meningioma with hyperostosis of the sphenoid wing
These images are of a patient who had a slowly progressive proptosis.
On the T2W-image the hyperostosis of the right sphenoid wing is seen, which corresponds to the CT-image.
Notice the small extra-axial lesion (arrow).
This is a meningioma.
On the coronal T1W-image post Gadolineum you can see the enhancement of the meningioma.
When a menigioma grows like this along the neurocranium, it is also called a meningioma en plaque.
Lacrimal gland lesions
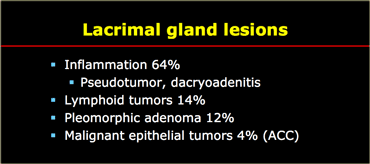
Lacrimal gland lesions are listed in the table on the left. Inflammatory conditions are by far the most common lesions of the lacrimal gland (i.e. Sj?gren's, TB, fungus, pseudotumor). These conditions do not cause masses.
The most common mass of the lacrimal gland is lymphoma followed by pleomorphic adenoma. Epithelial tumors including adenoid cystic tumors are uncommon.
Vascular Malformations
Vascular malformations can be intraconal, extraconal or multicompartment and that is the reason why they are not discussed in the categories above.
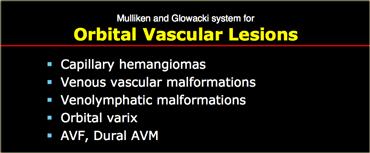
Before we show you some cases, we have to discuss the
Mulliken and Glowacki system for the categorization of vascular anomalies in the head neck region, which is widely accepted now.
Capillary hemangioma
The first lesion in the Mulliken & Glowacki system is the capillary hemangioma.
Capillary hemangiomas have the following characteristics:
- A true tumor with a growth phase 6-12 mos of age and involutional phase at 5-7 years of age.
- Mostly located in the skin, but also seen in the extraconal compartment of the eye.
- Usually regresses spontaneously, but sometimes it is treated with steroids, laser or interferon.
- Can be part of the PHACE-syndrome: Posterior fossa malformations, Hemangiomas, Arterial anomalies, Cardiac malformation and Eye abnormalities such as coloboma, glaucoma.
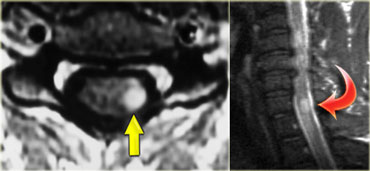
Venous Vascular Malformation
The second lesion in the Mulliken & Glowacki system is the venous vascular malformation.
On the left an image of a venous vascular malformation.
There is a lesion in the intraconal compartment with a phlebolith.
Most are unilocular, but this one is multilocular.
Venous vascular malformations have the following characteristics:
- The most common intraconal mass in an adult
- Most commonly seen in women, mean age 45 yrs, with slow progressive enlargement
- It is also known as a cavernous malformation, but this term should not be used any longer
- This lesion is characterized by phleboliths and can be part of Maffucci and Blue Rubber Bleb syndromes
- You can observe them, but usually they will grow over time and may need surgery
 Lymphatic malformation with fluid-fluid levels locaed both in the intraconal and in the extraconal compartment.
Lymphatic malformation with fluid-fluid levels locaed both in the intraconal and in the extraconal compartment.
Lymphatic malformations
The next entity is the lymphatic or veno-lymphatic malformation.
These are little cystic areas, that often bleed after minor trauma.
They may have high signal intensity on T1WI due to high protein or hemorrhage.
they usually do not enhance unless there is a venous component, that may show enhancement.
This lesion is in the 'family' of cystic hygroma.
More characteristics are:
- Childhood onset (60% before 16 y/o)
- May abruptly hemorrhage resulting in fluid-fluid levels
- May be extraconal or multicompartmental
- Association with intracranial malformations as in Turner's or foetus alcohol syndrome
- Absence of contrast enhancement in pure lymphatic lesions
Orbital varix
On the left images of a patient with an orbital varix, who had noticed that during straining there was a propulsion of the left eye . The upper image is during rest and the lower image is during valsalva at the moment of sneezing. During valsalva the varix shows extreme dilation (red arrow). Notice that during valsalva also on the normal side the superior ophthalmic vein dilates (blue arrow).
Conclusion
Important issues to remember are:
- How to distinguish between orbital and periorbital cellulitis.
- In a globe rupture, do not just look at the vitreous to see if it's flat, but look at the anterior chamber as well.
- Distinction between retinal and choroidal detachment .
And think of VITAMIN C and D
- Vascular: Varix and hemangioma
- Infectious: Subperiosteal abscess and orbital cellulitis
- Traumatic: Hyphema, detachments
- Acquired: Thyroid eye disease, sphenoid wing dysplasia
- Metabolic: Thyroid eye disease
- Idiopathic: Pseudotumor, Sarcoidosis, Devic's syndrome
- Neoplastic: Retinoblastoma, Melanoma, Perineural spread, Optic nerve meningioma and glioma
- Congenital: Coloboma, SOD, Retinoblastoma, NFBT
- Drugs: Chloramphenicol, Ethambutol
Charity
All the profits of the Radiology Assistant go to Medical Action Myanmar which is run by Dr. Nini Tun and Dr. Frank Smithuis sr, who is a professor at Oxford university and happens to be the brother of Robin Smithuis.
Click here to watch the video of Medical Action Myanmar and if you like the Radiology Assistant, please support Medical Action Myanmar with a small gift.