Meniscal pathology
David Rubin and Robin Smithuis
Radiology department of the Washington University School of Medicine, St. Louis, USA and the Rijnland hospital in Leiderdorp, the Netherlands
Publicationdate
This article is based on a presentation by David Rubin and adapted for the Radiology Assistant by Robin Smithuis.
Interactive cases are presented in the menu bar to test your knowledge.
by David Rubin and Robin Smithuis
Normal Meniscal Anatomy
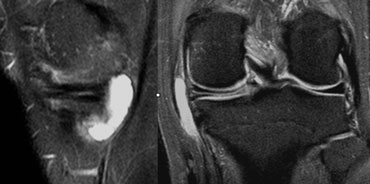
Medial meniscus
Both horns are triangular in shape and have very sharp points.
The posterior horn is always larger than the anterior horn (figure).
If this is not the case, then the shape is abnormal, which can be a sign of a meniscal tear or a partial meniscectomy.
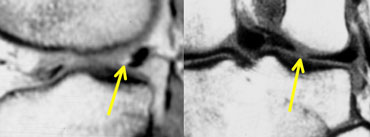
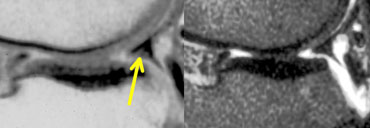
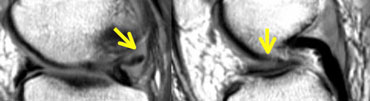
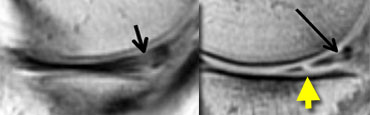
 LEFT: normal medial meniscal root immediately anterior to the posterior cruciate ligament. RIGHT: missing posterior root due to meniscal root tear.
LEFT: normal medial meniscal root immediately anterior to the posterior cruciate ligament. RIGHT: missing posterior root due to meniscal root tear.
The posterior root is immediately anterior to the posterior cruciate ligament.
If it is missing on the sagittal images, then there is a meniscal root tear (figure).
The anterior horn has an insertion on the tibia and a second portion that travels from medial to lateral to connect to the anterior horn of the lateral meniscus (intermeniscal or transverse ligament).
Lateral meniscus
On sagittal images the posterior horn is higher in position than the anterior horn.
Both horns are about the same size.
The lateral meniscus posteriorly comes up high over the tibial spine to insert near the posterior cruciate ligament.
This upward position of the posterior horn may be the reason for the higher signal intensity of the posterior horn in all planes due to magic angle effect.
Meniscal tears
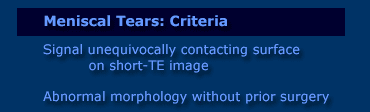
Criteria for tears
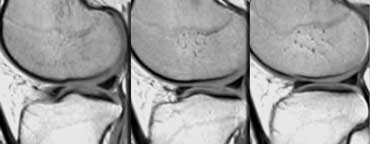
The two most important criteria for meniscal tears are an abnormal shape of the meniscus and high signal intensity unequivocally contacting the surface on PD images.
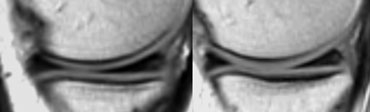
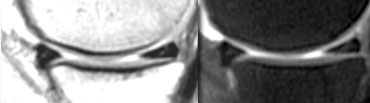
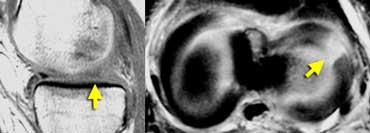
 High signal intensity not unequivocally contacting surface. Small black line on inferior margin of the meniscus. At arthroscopy the meniscus was normal.
High signal intensity not unequivocally contacting surface. Small black line on inferior margin of the meniscus. At arthroscopy the meniscus was normal.
It is a misunderstanding that menisci should be homogeneously low in signal intensity on proton-density images.
The meniscus does not have to be black.
Only when the high signal unequivocally reaches the surface of the meniscus you can make the diagnosis of a tear.
If there is doubt whether the high signal touches the surface, look at all the adjacent images.
If there is still doubt, then do not diagnose a tear.
If you have a questionmark in your head, say "meniscus is normal". (figure)
Nomenclature of Meniscal Tears
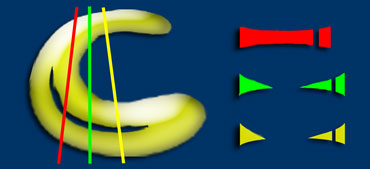
Shapes. There are 3 basic shapes of meniscal tears: longitudinal, horizontal and radial.
Complex tears are a combination of these basic shapes.
Displaced Tears
Bucket-handle tear = displaced longitudinal tear.
Flap tear = displaced horizontal tear.
Parrot beak = displaced radial tear.
Longitudinal, horizontal and radial tears
Longitudinal tears
Longitudinal tears parallel the long axis of the meniscus dividing the meniscus into an inner and outer part.
Therefore, the distance between the tear and the outer margin of the meniscus is always the same (figure).
The tear never touches the inner margin.
Longitudinal tears follow the collagen bundles that parallel the contour of the meniscus.
If a longitudinal tear has other components (horizontal or radial), then it is a complex tear violating the collagen bundles.
This requires a higher energy trauma.
 LEFT: abnormal shape of posterior horn. A piece is missing. RIGHT: displaced fragment in the intercondylar fossa.
LEFT: abnormal shape of posterior horn. A piece is missing. RIGHT: displaced fragment in the intercondylar fossa.
Longitudinal tear (2)
Bucket handle tear
is a displaced longitudinal tear.
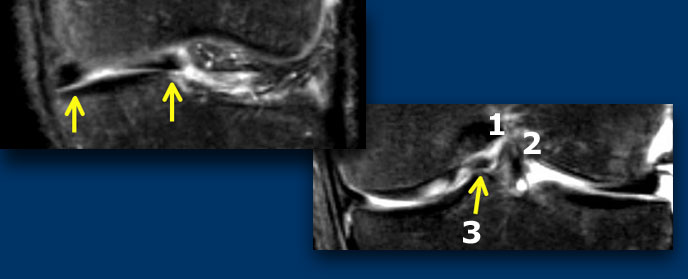 LEFT: meniscus is abnormal in shape and there is a displaced fragment. RIGHT: Three structures in the intercondylar fossa: post cruciate lig (1), ant cruciate lig (2) and displaced fragment (3).
LEFT: meniscus is abnormal in shape and there is a displaced fragment. RIGHT: Three structures in the intercondylar fossa: post cruciate lig (1), ant cruciate lig (2) and displaced fragment (3).
On coronal images bucket handle tears are easier to recognize.
Normally there are only two structures in the intercondylar fossa: the anterior and posterior cruciate ligament.
Any other structure in the intercondylar fossa is abnormal and a displaced meniscal fragment is the most likely possibility.
 Flipped meniscus: posterior horn is missing because it is flipped over and located on top of the anterior horn.
Flipped meniscus: posterior horn is missing because it is flipped over and located on top of the anterior horn.
Longitudinal tear (3)
Flipped meniscus is a form of bucket handle tear.
There is a capsular detachment or peripheral tear of the meniscus, usually the posterior horn.
The posterior horn flips over onto the anterior horn.
Horizontal tears
Horizontal tears divide the meniscus in a top and bottom part (pita bread).
If horizontal tears go all the way from the apex to the outer margin of the meniscus, they may result in the formation of a meniscal cyst.
The synovial fluid runs peripherally through the horizontal tear and accumulates within the meniscus and finally result in a cyst.
The connection with the joint space is often lost, so they will not fill with contrast on MR-arthrography.
The synovial fluid is absorbed and is replaced by a gelatinous substance.
There are 3 criteria for the diagnosis of a meniscal cyst:
- Horizontal tear.
- Fluid accumulation with bright signal on T2.
- Flat lining against the periphery of the meniscus.
The diagnosis of a meniscal cyst is important to the surgeon because it takes one operation on the outside of the knee to remove the cyst and another operation on the inside for the meniscus.
Radial tears
Radial tears are perpendicular to the long axis of the meniscus.
They violate the collagen bundles that parallel the long axis of the meniscus.
These are high energy tears. They start at the inner margin and go either partial or all the way through the meniscus dividing the meniscus into a front and a back piece.
Radial tears are difficult to recognize. You have to combine the findings on sagittal and coronal images to make the diagnosis.
The following combination of findings is diagnostic:
In one plane: triangle missing the tip and in the other plane: a disrupted bow tie.
Small radial tears are difficult to diagnose.
Sometimes the only sign is a disrupted bow tie.
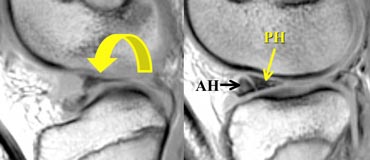
 LEFT: Absent or empty meniscus on sagittal image.RIGHT: Axial image shows complete radial tear leading to a defect in the meniscus.
LEFT: Absent or empty meniscus on sagittal image.RIGHT: Axial image shows complete radial tear leading to a defect in the meniscus.
If you image a complete radial tear directly along the length of the tear you will see an absent or empty meniscus.
These complete radial tears open up and give the impression that there is a part missing.
However you will not find a displaced meniscal fragment. It is simply separation of the meniscal parts.
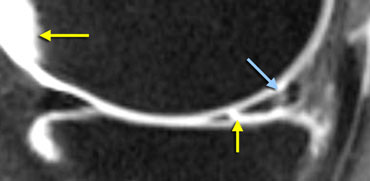
 Meniscal root tear: on sagittal images there is an absent or empty meniscus-sign adjacent to the posterior cruciate ligament where the meniscal root should be. On coronal images a meniscal root tear is confirmed.
Meniscal root tear: on sagittal images there is an absent or empty meniscus-sign adjacent to the posterior cruciate ligament where the meniscal root should be. On coronal images a meniscal root tear is confirmed.
Meniscal root tear
A meniscal root tear is a radial tear located at the meniscal root.
Normally when you image the posterior cruciate ligament on sagittal images you should see a considerable portion of the posterior horn of the meniscus on that image or the image adjacent to it.
If this is not the case it is an absent or empty meniscus-sign, indicating a radial tear.
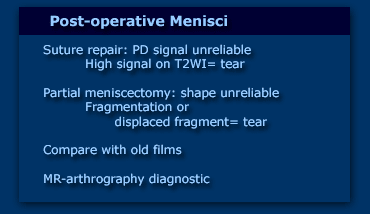
Post-operative meniscus
Post-operative menisci are harder to evaluate because the two most important criteria, i.e. abnormal signal and abnormal shape, do not apply.
Abnormal signal is no longer a reliable sign of a tear, because if there has been a suture repair, this will heal with scar tissue, which also has high signal on PD-images (figure).
Although an uncommon finding, if there is also high signal on T2-weighted images, then you can make the diagnosis of a tear, as this is the result of synovial fluid leaking into a meniscal tear.
This however is an uncommon finding.
Abnormal shape can be the result of partial meniscectomy.
So you need to know what procedure was performed during arthroscopy.
Only when comparison is made with prior postoperative images, can you determine, if an abnormal shape is a new finding indicative of a new tear.
Sometimes differentiation between normal post-op findings and a re-tear is not possible on conventional MR-images.
In these cases, MR-arthrography with 40cc diluted Gadolinium helps to make the distinction because even small amounts of Gadolinium that leak into a tear are readily visible on fat saturated T1 images.
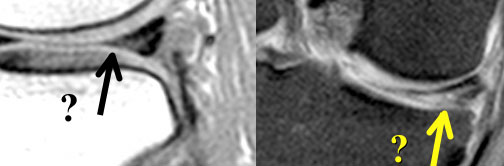
Post-operative Meniscus 1
The case on the left shows a meniscus with an abnormal shape aswell as abnormal signal touching the surface on PD but not on T2W-images.
This patient had a prior partial meniscectomy and a suture repair.
On the basis of these imaging findings, it is impossible to tell if this is a tear or a normal postoperative finding.
This patient had another operation for ACL reconstruction.
The surgeon looked at the meniscus and the meniscus was found to be normal i.e. no tear.
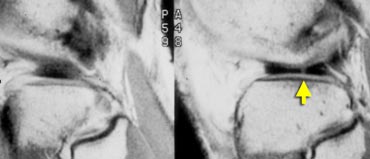
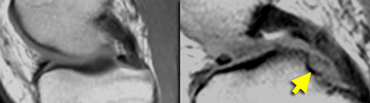
 LEFT: Old MR exam with tear. Patient had a suture repair. RIGHT: On new exam, there is a new tear (yellow arrow). It is not possible to tell if the old tear has healed.
LEFT: Old MR exam with tear. Patient had a suture repair. RIGHT: On new exam, there is a new tear (yellow arrow). It is not possible to tell if the old tear has healed.
Post-operative Meniscus 2
This patient had a suture repair for meniscal tear.
There was a new injury.
On the new MR, it is impossible to determine if the old tear had healed.
However a new tear is seen, so this case is easy.
 MR-arthrogram: In the new tear the signal is as bright as in the synovial fluid (yellow arrows). In the healed tear the signal is not as bright.
MR-arthrogram: In the new tear the signal is as bright as in the synovial fluid (yellow arrows). In the healed tear the signal is not as bright.
On an MR-arthrogram, there was very high signal intensity in the new tear comparable with the synovial fluid, but only moderate signal intensity at the healed old tear.
So comparison with the old films was diagnostic for the new tear, while the arthrogram showed that the old tear has healed.
Post-operative Meniscus 3
This patient also had a suture repair for meniscal tear.
After a new injury, the PD-images show high signal unequivocally reaching the surface of the meniscus (seen on the original films, but not clearly seen on the compressed image on the left).
On this image, it is not possible to tell if the tear has healed.
So an MR-arthrogram was performed which showed that the tear has healed.