Arthritis
Laurens van Baardewijk, Frank Looijmans, Frank Smithuis and Matthieu Rutten
Máxima MC, Cooperative Lumirad U.A., Amsterdam University Medical Center, Jeroen Bosch Hospital and Radboud University Medical Center in The Netherlands
Publicationdate
In this article we provide an overview of the different imaging findings of common joint diseases as a useful tool in daily musculoskeletal radiology.
Arthritis is a challenging topic. A long list of diagnoses has to be considered when looking at X rays of the hand and feet, each with its own extensive set of findings.
Sometimes the abnormalities are pathognomonic for a specific disease, but more often the findings are non-specific because there is a lot of overlap between different joint diseases.
When you start looking at arthritis cases, remember the following:
- If it is the first examination, then try to make a differential diagnosis based on imaging findings as well as patient information and lab findings.
- Master yourself in diagnosing osteoarthritis and rheumatoid arthritis and remember the distinct features between these two entities.
- If it is not typical osteoarthritis or rheumatoid arthritis, then use the systematic approach in the first paragraph.
- If it is a follow up case, then check disease progression and look for new erosions. Remember that secondary osteoarthritis can develop. Secondary osteoarthritis can also be a sign of lowgrade progression of the original disease.
You can click on all images for an enlarged view.
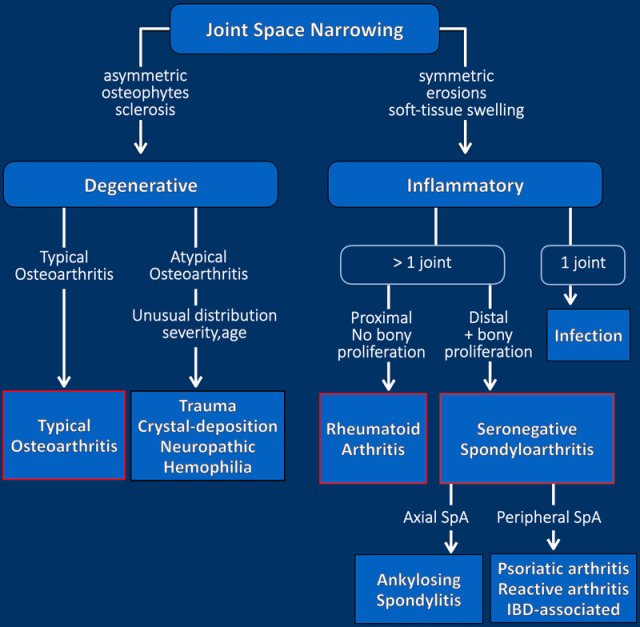
Systematic Approach
This flow chart shows the approach to the radiographic evaluation of arthritis. In the presence of joint space narrowing, it is important to differentiate degenerative from inflammatory conditions.
Degenerative joint disease
This is characterized by osteophytes and subchondral sclerosis with an asymmetric distribution both when you compare left and right as well as within the joint itself. Usually it is typical osteoarthritis.
When findings are atypical (unusual combination of age, affected joint and severity) think of posttraumatic, CPPD, neuropathic or rare diseases like hemophilic arthritis.
Inflammatory joint disease
This is characterized by bone erosions, osteopenia, soft-tissue swelling and uniform, symmetric joint space loss.
Inflammation of a single joint should raise concern for infection.
Multiple symmetric joint inflammation in a proximal distribution in the hands or feet without bone proliferation suggests rheumatoid arthritis.
When the inflammation is more in a distal distribution in the hands or feet with bone proliferation it suggests a seronegative spondyloarthropathy (SpA).
SpA is a group of chronic inflammatory diseases associated with HLA-B27 (2).
Axial SpA - most commonly ankylosing spondylitis - is located more in the axial skeleton.
Peripheral SpA - like psoriatic, reactive and IBD-associated arthritis - is located more in the peripheral skeleton.
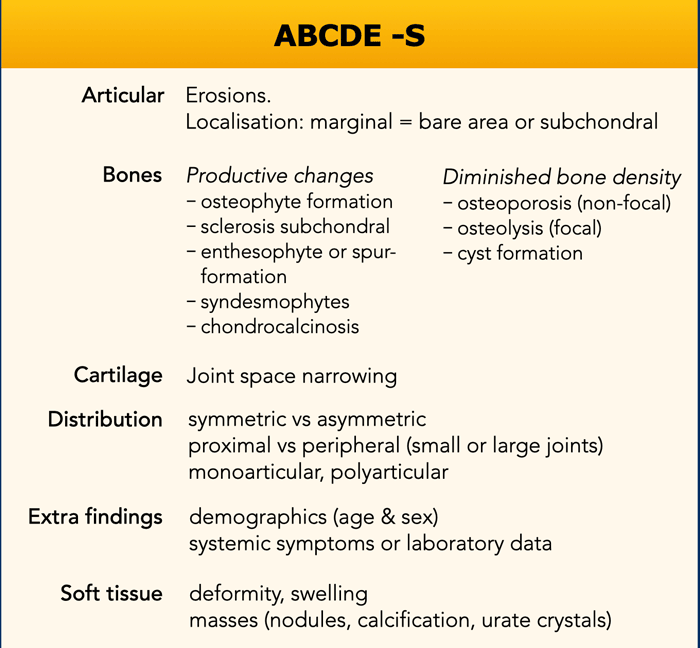
ABCDE-S
Joint diseases have variable manifestations with an overlap of radiological features.
The ABCDE-S mnemonic is a helpful tool for a systematic and complete radiological interpretation and reporting.
We use the ABCDE-S, which stands for Articular, Bone, Cartilage, Distribution, Extra's and Soft tissue.
There are variants of this mnemonic. Some use ABCDE for Alignment, Bone, Cartilage, Distribution and Effusion.
Articular - erosions
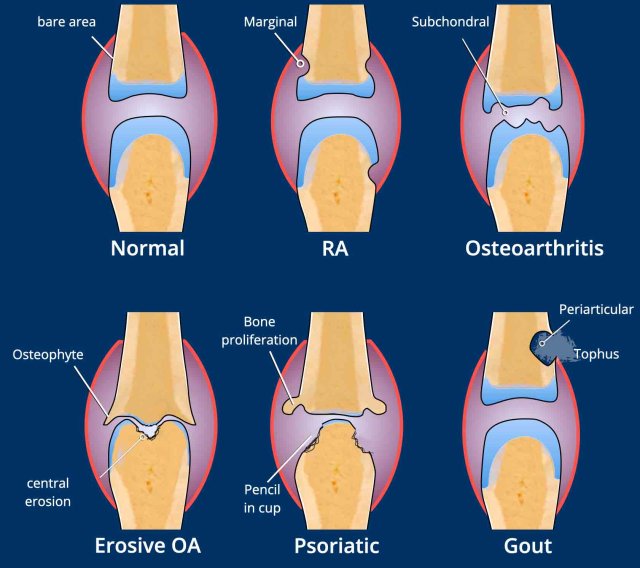
Marginal erosions
They occur at the bare area of the joint, where the bone is not covered by articular cartilage. They are typically seen in rheumatoid arthritis (MCP-joints) and psoriatic arthritis (DIP).
Subchondral erosions
They occur at the subchondral bone plate of the articular surfaces. They are a typical feature of erosive osteoarthritis.
Gullwing deformity
In erosive osteoarthritis the combination of central erosions and osteophytes results in a gullwing deformity.
Pencil-in-cup deformity
In psoriatic arthritis the combination of marginal erosions and bone proliferation can result in a pencil-in-cup deformity.
Peri- or juxtaarticular erosions.
Gout erosions are a bit more eccentric juxta-articular located, where the joint capsule attaches to the bone. They are most often seen in the MTP1-joint.
Typical examples of specific erosion patterns
- Rheumatoid arthritis.
Typical marginal erosions in MCP-joints. - Erosive osteoarthritis.
Subchondral erosions in DIP- and PIP-joints. The concurrent formation of osteophytes results in a gull-wing deformity. - Gout.
Eccentric erosion with an overhanging edge. The sclerotic margin in this case indicates chronic and indolent disease. - Infection.
Destructive changes with cartilage loss and erosions. - Psoriatic arthritis.
Bony erosions narrowed the end of the proximal phalange as a “pencil”, which rests in the “cup” formed by the expanded base of the distal phalanx as a result of bony proliferations. - Scleroderma.
And other multisystem disorders can produce erosions at the distal tufts, this is called acro-osteolysis.
Alignment
Some use the A of ABCDE-S for Alignment.
The problem however is that misalignment or malalignment can be seen in all end-stage joint diseases, whether it is degenerative or inflammatory.
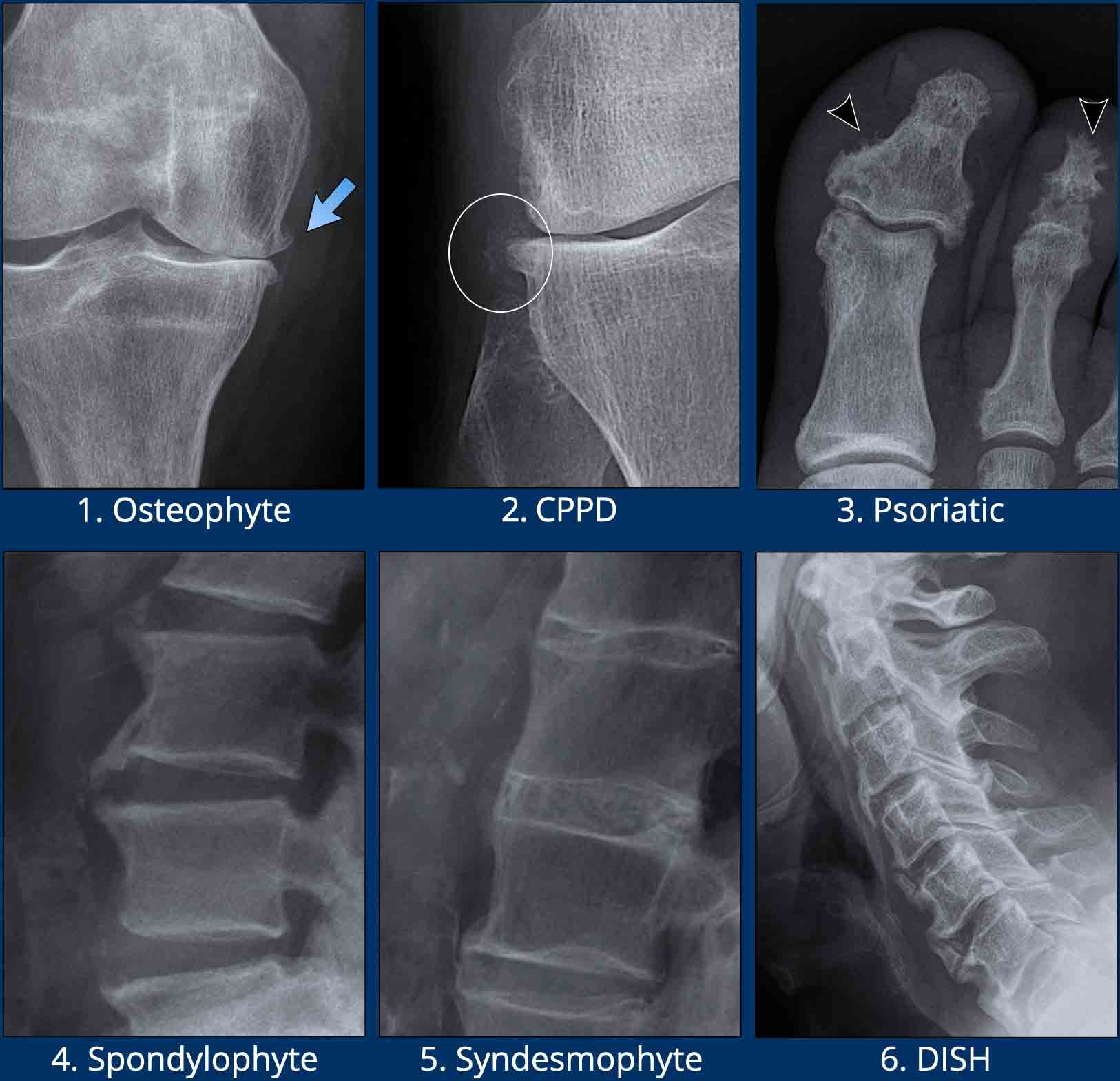
Bone - formation
Bone formation or proliferation is seen in many joint diseases and especially in osteoarthritis, DISH and spondyloarthritis like ankylosing spondylitis and psoriatic arthritis.
It is NOT present in the active phase of rheumatoid arthritis.
Images
- Osteophytes in osteoarthritis.
Bony proliferations, that develop at the margins of a synovial joint secondary to articular cartilage damage in osteoarthritis. - Osteophytes in a patient with CPPD.
Notice the soft tissue calcifications (circle). - Bony proliferations in Psoriatic arthritis.
Sometimes described as fluffy periostitis (arrowheads). - Spondylophytes
Osteophytes in the spine in spondylosis / degenerative disease. Typical orientation is horizontal / perpendicular to the spine. - Syndesmophytes
Paravertebral ossifications in the ligaments of the spine. Typical orientation is vertical / parallel to the spine. This is the hallmark of ankylosing spondylitis. - DISH
Ossification in the anterior longitudinal ligament. These ossifications are more bulky compared to ossifications in ankylosing spondylitis.
Bone - density
Bone density changes either present as osteopenia or as osteosclerosis.
Periarticular osteopenia (figure) is typically seen in rheumatoid arthritis and not in osteoarthritis. Peri-articular demineralization develops as a result of the hyperemia of the inflamed synovium and soft tissues.
Subchondral sclerosis is typically seen in osteoarthritis. Also in patients with neuropathic arthritis.
Images
Here two examples of periarticular osteopenia in patients with rheumatoid arthritis.
The osteopenia can be very subtle.
It may help to play with the window width settings (detail views in the center) or to look through your eyelashes to see the osteopenia.
Cartilage
Degenerative diseases affect the cartilage non-uniformly or asymmetrically, since this is the result of mechanical load, which is not evenly distributed throughout the joint.
Inflammatory diseases affect the cartilage uniformly, since the synovitis is present in the entire joint.
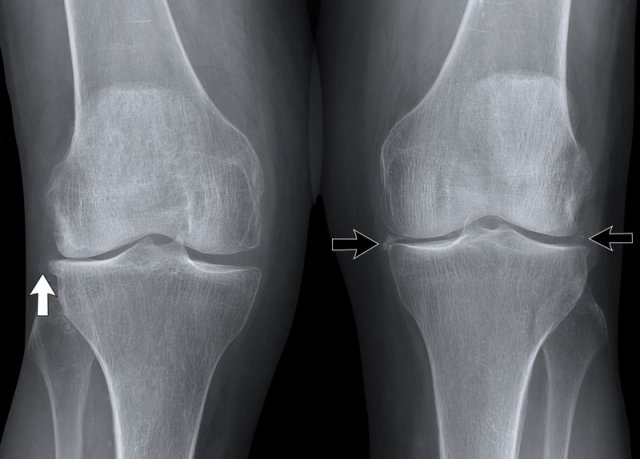
- Typical osteoarthritis with cartilage loss on the medial side, subchondral sclerosis and osteophytes.
- There is uniform cartilage loss.
There are no osteophytes.
In such a case your first thought should be inflammatory joint disease.
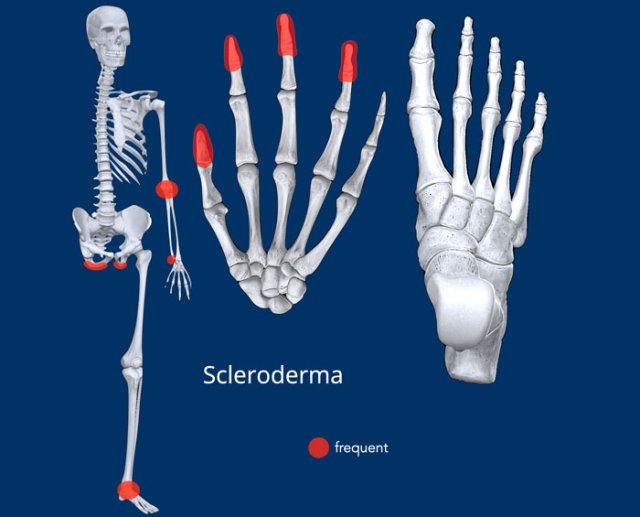
Distribution
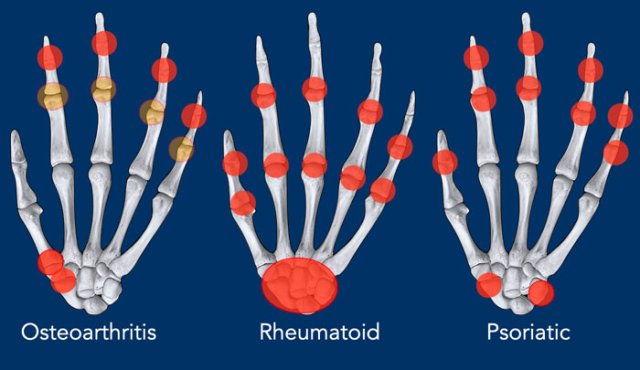
Understanding distribution patterns is a very powerful tool, since most common diseases (osteoarthritis, rheumatoid and psoriatic arthritis) have distinctive patterns.
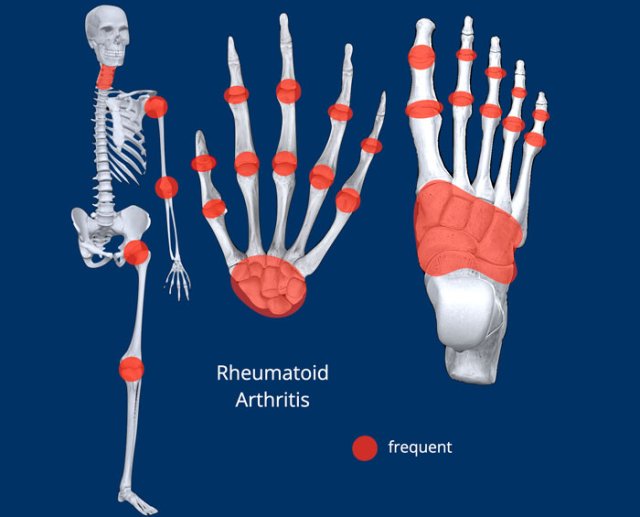
In the following chapters on the various joint diseases, we will start each chapter with an illustration of the distribution.
Distribution in the hands
- Osteoarthritis is located in CMC1-, STT- and DIP-joints.
- Rheumatoid arthritis is located mainly in the carpus and MCP- (and PIP-) joints. Also, the processus styloideus ulna is an often affected area.
- Psoriatic arthritis is located more distally in PIP and DIP joints. In the wrist the STT and triquetrohamate joints are common locations aswell.
Extra findings
Serological tests can help when rheumatic diseases are suspected.
A positive rheumatoid factor (RF) or anti-citrullinated peptide (CCP) antibody test can support the diagnosis when rheumatoid arthritis is suspected.
A positive HLA-B27 test can aid establishing a diagnosis of ankylosing spondylitis (AS).
Nonspecific inflammatory markers, including the erythrocyte sedimentation rate (ESR) and the C-reactive protein (CRP), are often elevated in any inflammatory disease.
However, immunologic tests are not always helpful, since they have limited specificity.
Soft tissue
Soft tissue swelling and calcifications are frequently seen in arthritis and can help to narrow the differential diagnosis.
- Chondrocalcinosis is a descriptive term for fine calcifications within a joint. Although not very specific, CPPD is very likely when chondrocalcinosis is located around the TFCC, radiocarpal joint or within the knee joint.
CPPD can cause SL dissociation (left arrow). - Chondrocalcinosis in the knee joint.
- Mild radiopaque nodular soft tissue swelling next to the MTP1 joint is almost pathognomonic for gout. Other typical locations are tendon insertions around the knee, for example the popliteus tendon, or flexor tendons in the ankle joint.
- Fusiform periarticular soft tissue swelling is a common finding in psoriatic arthritis and may involve the entire digit resulting in dactylitis or a "sausage-digit". Notice the pencil-in-cup deformity of the joint.
- Coarse calcifications in the subcutaneous tissue surrounding distal ends of fingers or toes are very likely caused by scleroderma.
- Scleroderma
- Heberden noduli, due to osteophytes in osteoarthritis
- Rheuma noduli. These soft tissue nodules are too big for Heberden noduli and there are no osteophytes.
- Chondrocalcinosis in CPPD. Again, SL dissociation is seen, with severe secondary degeneration. This severe degeneration is called a SLAC wrist, which stands for Scaphoid Lunate Advanced Collapse.
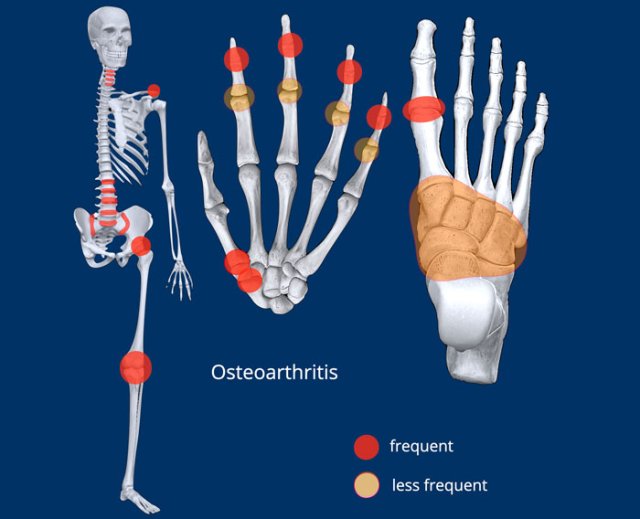
Osteoarthritis
Key findings
Non-uniform joint space narrowing with osteophytes, most often in weight-bearing joints. No erosions.
Clinical
- Most common joint disease, incidence increases with age.
- Characterized by non-inflammatory destruction of cartilage.
- Primary idiopathic and secondary form (e.g., trauma, obesity)
Radiological findings
- Articular: no erosions
- Bone: no osteopenia. Productive changes like osteophyte formation and subchondral sclerosis.
- Cartilage: non-uniform joint space narrowing. Subchondral cyst formation (geode).
- Distribution: see illustration
- Extra findings: subluxations associated with hallux valgus or hallux rigidus
- Soft tissue: Heberden‘s nodes in DIP-joints or Bouchard’s node in PIP-joints.
Teaching point: Many arthropathies show secondary osteoarthritis in a later stage.
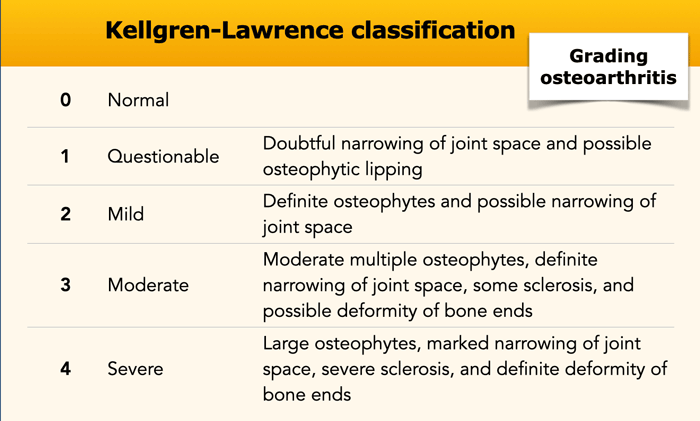
In the knee, osteoarthritis is classified by the Kellgren and Lawrence classification.
This classification can be used when grading degeneration in other joints, but it is primarily designed for the knee.
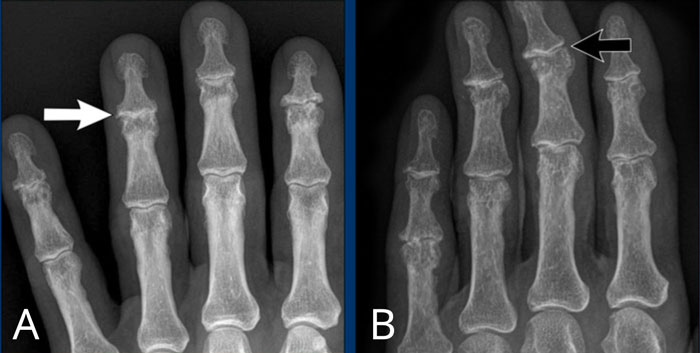
A
Joint space narrowing of the 4th DIP joint (arrow) with osteophyte formation and subchondral sclerosis.
B
Asymmetric joint space narrowing of the 2-5th DIP joint with osteophyte formation, subchondral sclerosis and slight ulnar deviation of the 3th DIP joint (arrow).
The PIP joints are also affected, but less severe.
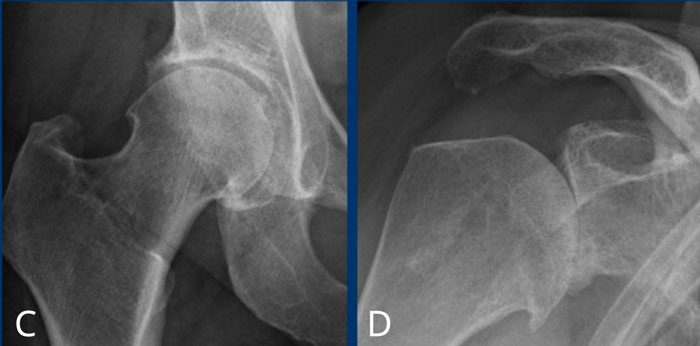
C
Slight narrowing of the cranial joint space of the hip joint at the right side with osteophyte formation and subchondral sclerosis (Kellgren-Lawrence classification grade 3).
D
Severe narrowing of the glenohumeral joint space with osteophyte formation and subchondral sclerosis (Kellgren-Lawrence classification grade 4).
E
Hip osteoarthritis
Severe non-uniform narrowing of the hip joint with osteophyte formation, subchondral sclerosis and large cyst formation.
In these later stages, joint deformity with broadening and deformation of the femoral head can occur.
F
Knee osteoarthritis
Moderate to severe asymmetric narrowing of the medial compartment of the femorotibial joint space with osteophyte formation and subchondral sclerosis (Kellgren-Lawrence classification grade 3-4).
G
CMC1 osteoarthritis
Non uniform joint space narrowing of the CMC 1 joint with osteophyte formation and subchondral sclerosis.
There is a large subchonderal cyst in the base of the first metacarpal (white arrow).
H
STT osteoarthritis
Non uniform joint space narrowing of the scaphotrapeziotrapezoid (STT) joint with osteophyte formation and subchondral sclerosis.
This is a difficult case.
Dominant finding is non-uniform joint space narrowing in CMC and DIP joints. So this patient has osteoarthritis. The severity of findings may suggest erosive osteoarthritis.
However, there is also joint space narrowing of the MCP joints and a possible erosion in the lunate bone. Without abnormalities in the PIP joints it is very unlikely that these abnormalities are all due to osteoarthritis.
Most likely this patient has both rheumatoid arthritis and osteoarthritis.
Rheumatoid Arthritis
Key findings
Symmetrical uniform cartilage damage with marginal erosions predominantly in MCP-joints and the carpus, not in DIP-joints. No bone proliferation.
Clinical
- Usually starts to develop between the ages of 40 and 50.
- RF and anti-CCP are most often positive.
- Begins in the appendicular skeleton in a symmetrical pattern.
Radiological findings
- Articular: erosions, typically at the marginal area i.e. bone not covered with cartilage, deformities
- Bone: periarticular osteopenia. No bone production or proliferation in the active phase.
- Cartilage: uniform cartilage destruction.
- Distribution: see illustration, symmetric peripheral distribution.
- Extra findings: autoimmune inflammatory disease that affects many organs, such as the lungs, skin, eyes or the heart.
- Soft tissue: fusiform swelling, nodes, deformity
Typical marginal erosions and joint space narrowing of MCP 3-5.
Also note the uniform joint space narrowing of the MCP joints.
The PIP-joints only show minimal joint space narrowing.
This is a case with end stage rheumatoid arthritis with severe erosive changes and ligamentous ruptures causing dislocation of the MCP joints.
Scapholunate dissociation (white arrow) is a common finding due to diffuse carpal inflammation. Both the dissociation and inflammation can cause joint space narrowing in the radiocarpal joint.
Notice also the erosion in the distal ulna with surrounding soft tissue swelling (blue arrow).
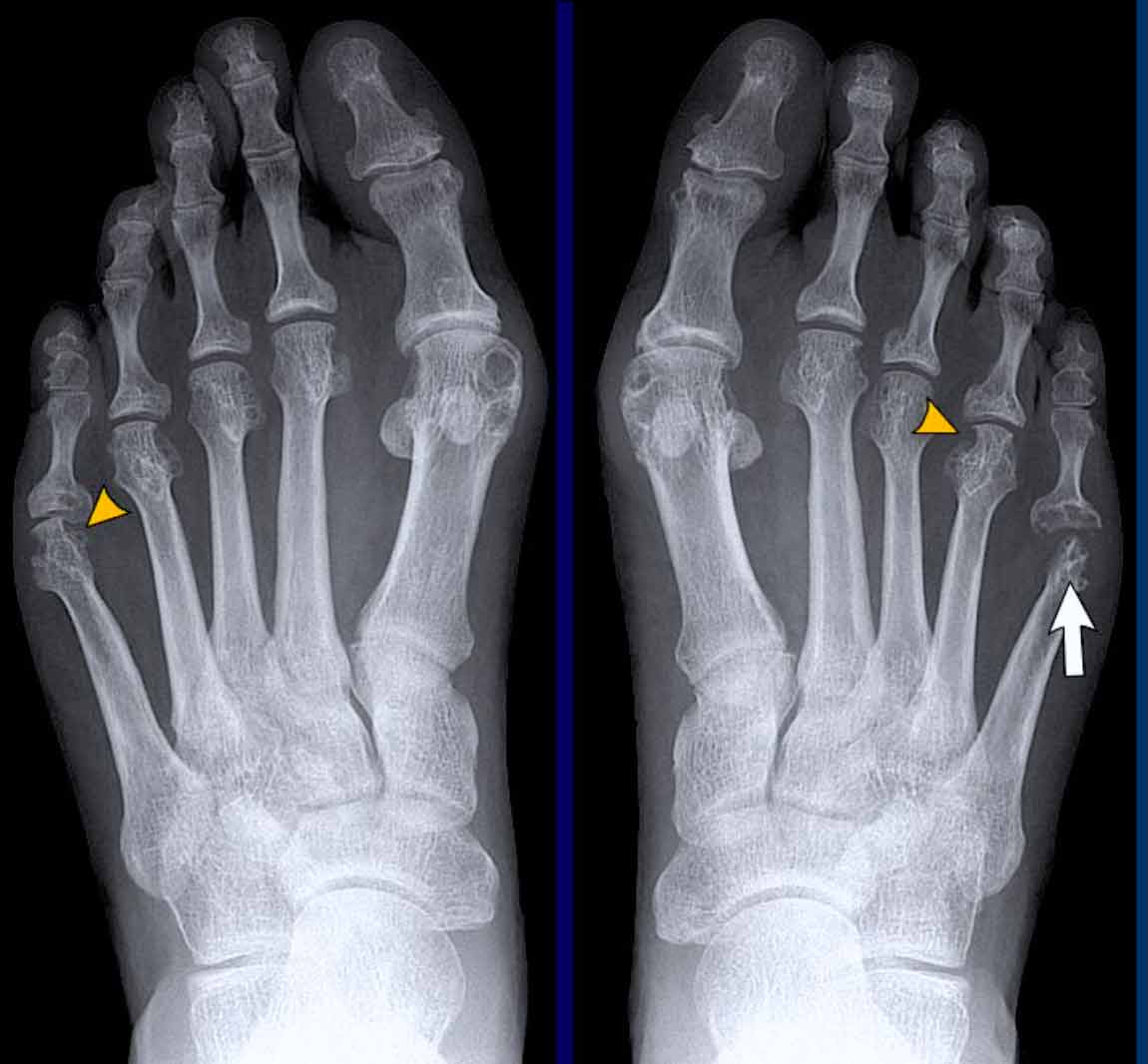
In this case of rheumatoid arthritis there are marginal erosions adjacent to almost all MTP joints (arrowheads).
The 5th MTP joint is most frequently involved in rheumatoid arthritis.
When erosions are as severe as in this case, it can look like pencil-in-cup deformity (white arrow) as is frequently seen in psoriatic arthritis.
However, the primarily affected MTP joints distribution and less affected interphalangeal joints is the clue that this is a case of rheumatoid arthritis.
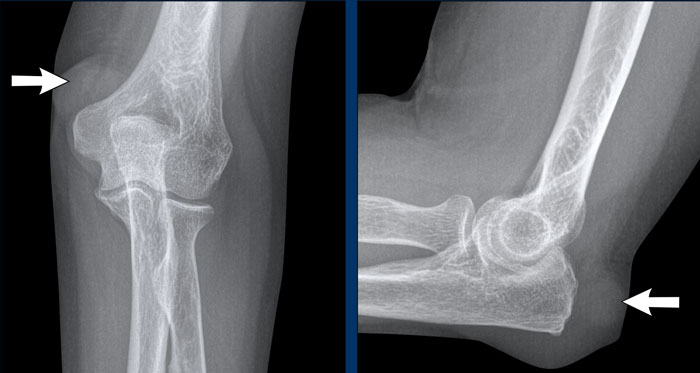
Rheumatoid nodules
Rheumatoid nodules are firm lumps that appear subcutaneously in up to 20% of patients with rheumatoid arthritis.
These nodules usually occur adjacent to overexposed joints that are subject to trauma or pressure, such as the fingers joints and elbows.
In this variant of rheumatoid arthritis, there are often no joint abnormalities.
Images
Soft tissue mass (i.e., rheumatoid nodules) in the subcutis at the dorsolateral side of the olecranon.
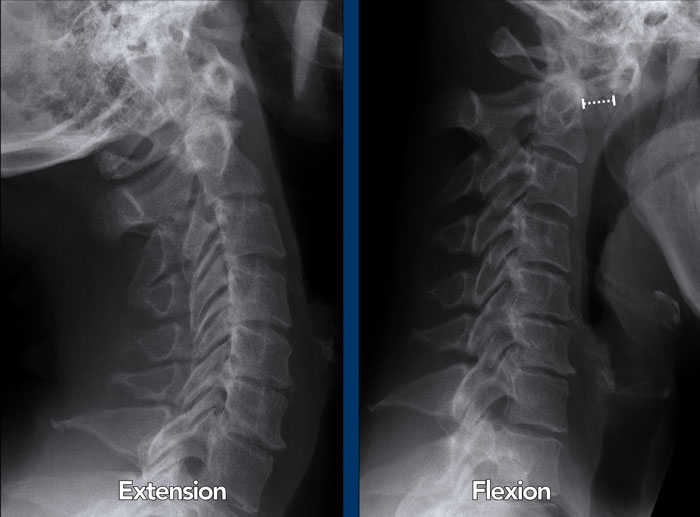
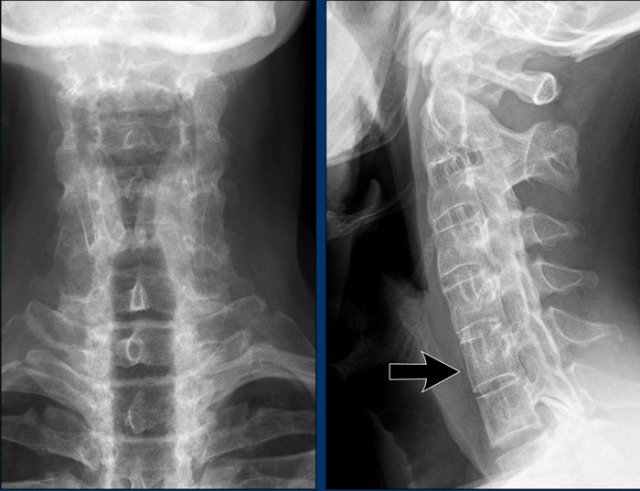
Atlanto-axial subluxation
The cervical spine is often affected in rheumatoid arthritis and can present as atlantoaxial instability, subaxial subluxation or basilar invagination with cranial settling.
Cranial settling occurs when the dens extends into the foramen magnum.
Atlanto-axial subluxation is an important and potentially life threatening complication of rheumatoid arthritis. It is defined when the space between the dens of C2 and the arch of the atlas exceeds more than 3 mm. It is caused by inflammatory ligamentous laxity.
Instability in this joint may result in numerous neurological symptoms due to compression of the spinal cord.
Images
In flexion of the cervical spine there is widening of the distance (14 mm) between the dens and the posterior surface of the anterior atlas ring (normal ≤3 mm).
Basilar invagination
Basilar invagination also called cranial settling or basilar impression occurs in 5-10% of patients with cervical rheumatoid arthritis.
In basilar invagination the odontoid is prolapsing into the foramen magnum limiting the space for the spinal cord.
Clinical presentations range from chronic headaches, limited neck motion to acute neurologic deterioration (spinal cord and brain stem compression, which can lead to paralysis or even death if the neck is moved in certain positions).
Images
Scroll through the CT-images.
There is upward migration of the odontoid process into the occipital foramen.
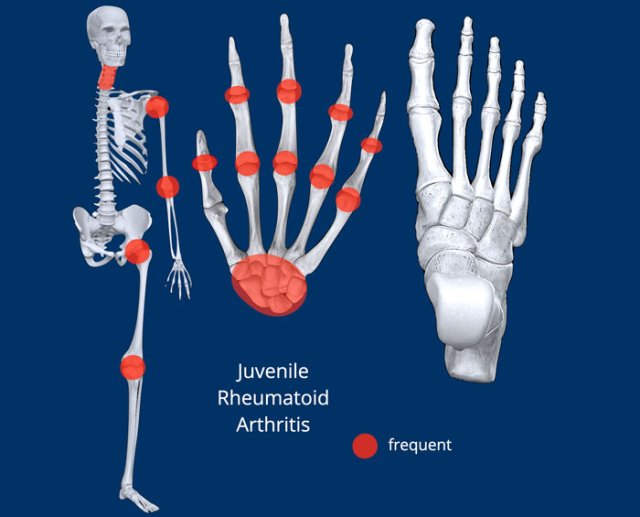
Juvenile Rheumatoid Arthritis
Key findings
Polyarthritis in the pediatric population with variable manifestations and radiographic findings.
Clinical
It starts before the age of 16 years.
Usually located in the larger joints.
Joint changes are distinct from adult RA, however the distribution can be similar.
Radiological findings
- Articular: erosions are late manifestations
- Bone: osteopenia, bone oedema, periosteal reaction. growth disturbances: epiphyseal overgrowth, early growth plate closure, contractions and ankylosis
- Cartilage: cartilage destruction and erosions are late manifestations
- Distribution: see illustration
- Extra findings: stills, uveitis, tendinitis, bursitis.
- Soft tissue: swelling, deformity
Juvenile rheumatoid arthritis is a diagnosis of exclusion, when inflammatory changes do not match other inflammatory diseases.
Juvenile rheumatoid arthritis is also called juvenile idiopathic arthritis.
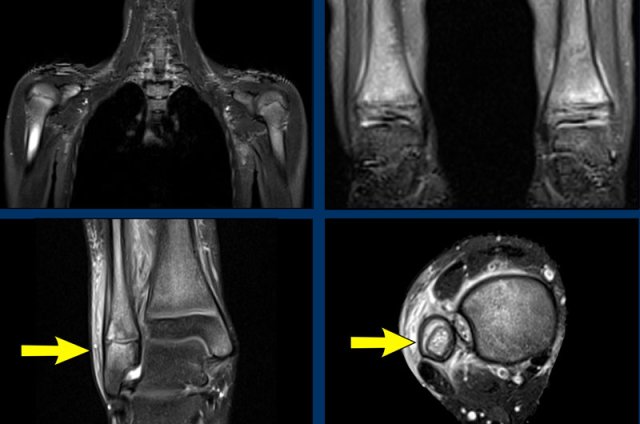
Image
Typical ankylosis of the carpal bones.
Periarticular osteopenia
In this patient with juvenile rheumatoid arthritis there are multiple erosions in the carpus and in the base of the metacarpal bones.
Diffuse joint space narrowing is present.
Continue with the MR of this patient.
MR-findings:
Diffuse effusion in all wrist joints.
Diffuse bone marrow edema in all carpal bones.
Erosions, for example in scaphoid, capitate and hamate.
Destruction of joint space and cartilage, most striking in STT and CMC4/5.
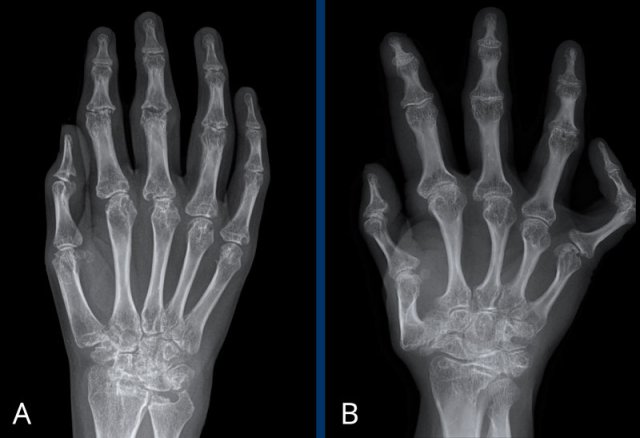
Two patients with juvenile rheumatoid arthritis
A. Multiple erosions affecting the carpal bones and MCP joints. Collapse of the scaphoid and lunate bone.
B. Adult with a history of juvenile arthritis. Abnormal bone length due to premature growth plate closure and epiphyseal overgrowth. Severe joint malalignment.
Both cases show periarticular osteopenia.
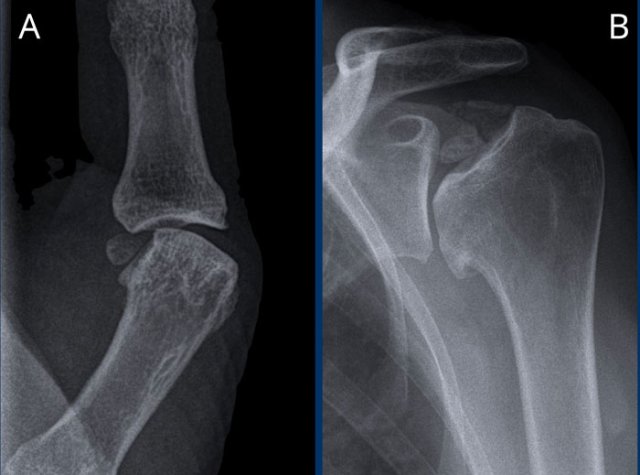
Large erosions of the humerus, glenoid and acromion in a patient with juvenile idiopatic arthritis.
Erosions and joint space narrowing of the right hip joint in a patient with juvenile idiopatic arthritis.
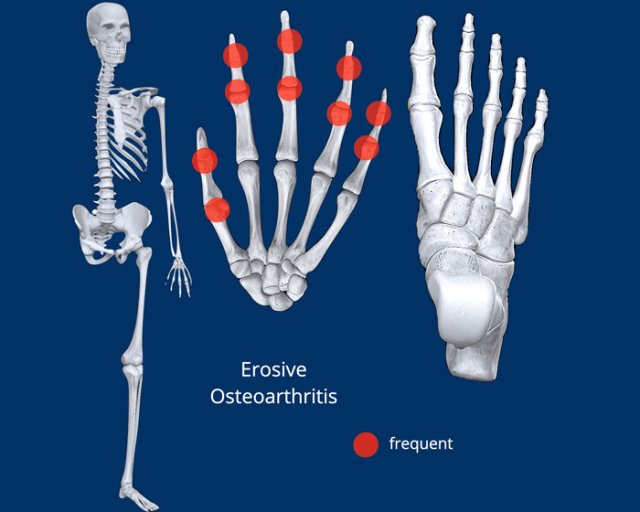
Erosive osteoarthritis
Key findings
Arthropathy with the age of onset and distribution of osteoarthritis, with an inflammatory and erosive component.
Clinical
- Inflammatory form of osteoarthritis of the hand
- Affects the DIP and PIP joints and the first carpometacarpal joint of the hand most frequently, just like osteoarthritis.
- The combination of osteofyt formation (like osteoarthritis) and central erosions, which causes a characteristic biconcave articular surface, is called the gullwing or seagull deformity. It can look like a pencil-in-cup deformity.
Radiological findings
- Articular: joint space narrowing
- Bone: sclerosis, productive bony changes with osteophyte formation, ankylosis
- Cartilage: subchondral central erosions
- Distribution: see illustration. Same distribution as with osteoarthritis, with a preference for the IP joints (DIP more than PIP)
- Extra findings: occurs primarily in postmenopausal women
- Soft tissue: rheumatoid arthritis-like proliferative intra articular synovitis, soft tissue swelling around the joint
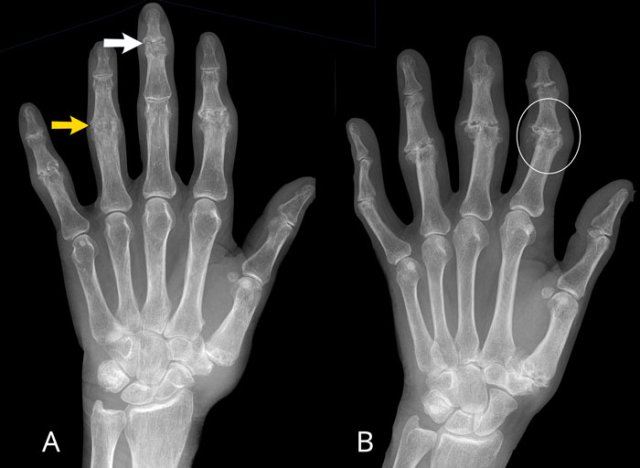
A
Erosive changes of PIP 2-5 and DIP 3-5.
Typical gullwing deformity in DIP 3 (white arrow).
Ankylosing of PIP 4 (yellow arrow), which occurs in a late phase of the disease.
B
Joint space narrowing with central erosions. Gullwing deformity of PIP 2-4, DIP 2 and CMC-1 joint.
Ankylosing of DIP 3. Medial deviation of PIP 2.
Ball catcher view of the hands in a patient with erosive osteoarthritis.
There is bilateral extensive damage to the IP joints.
Note the symmetrical distribution and sparing of the MCP joints.
Typical gull-wing appearance of the DIP-joints, also known as seagull erosions or sawtooth appearance.
This is classically seen in erosive osteoarthritis, but has also been reported in psoriatic and rheumatoid arthritis.
Septic arthritis
Key findings
Rapid destruction of one joint with extensive erosions and effusion.
Clinical
Septic arthritis, also called infectious arthritis, is usually an acute mono-arthritis.
It is secondary to bacteremia, local spread of infection or a complication of surgery or injection.
Septic arthritis leads to rapid joint destruction and requires prompt aspiration or drainage.
Radiological findings
- Articular: joint effusion sometimes with gas. thickened synovium, erosions.
- Bone: Early stage (after a few days): juxta-articular osteoporosis, followed by erosion and joint space narrowing. Adjacent bone marrow edema. End-stage: ankylosing and sclerosis.
- Cartilage: Late cartilage destruction
- Distribution: mono-arthritis. Most common in knees in adults and knees or hips in children (most common in infants up to 12 months).
- Extra findings: fever, bacteria in synovial fluid.
- Soft tissue: erythema, warmth and swelling. MRI shows thickened enhancing synovium. Outpouching of the synovium and microabscesses can be seen.
Images
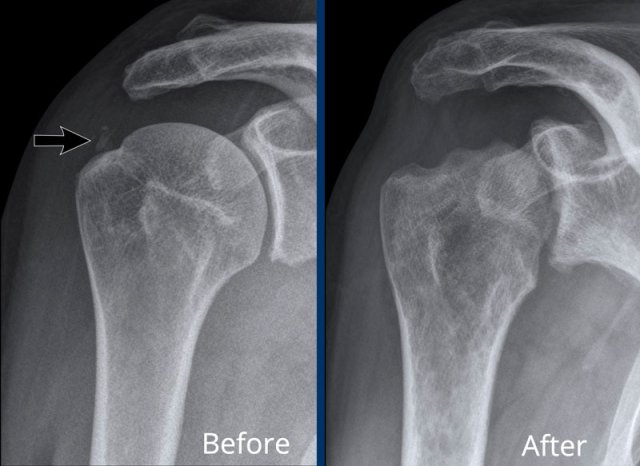
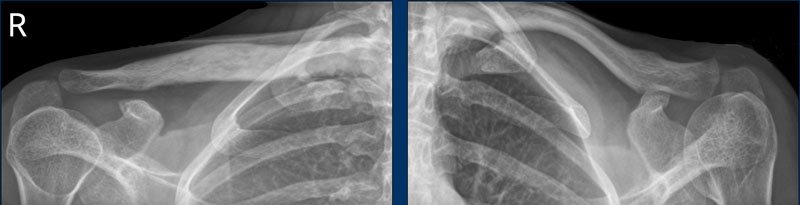
A. Soft tissue calcifications in the rotator cuff. Patient got a subacromial injection for relief of symptoms.
B. After corticosteroid injection severe cartilage loss in the glenohumeral joint and bone destruction of the humeral head occured. This was the result of a septic arthritis, which is a rare complication of injection.
Septic arthritis of the PIP 3-joint.
There is enormous soft tissue swelling of the 3rd finger.
There are extensive erosions of the joint with some small bone fragments.
Infectious arthritis as a compllication of a fingertip abscess.
The findings are:
- Soft tissue swelling
- Erosions and joint space narrowing of the DIP-joint.
- The subchondral sclerosis and osteophyte formation are caused by secondary osteoarthritis.
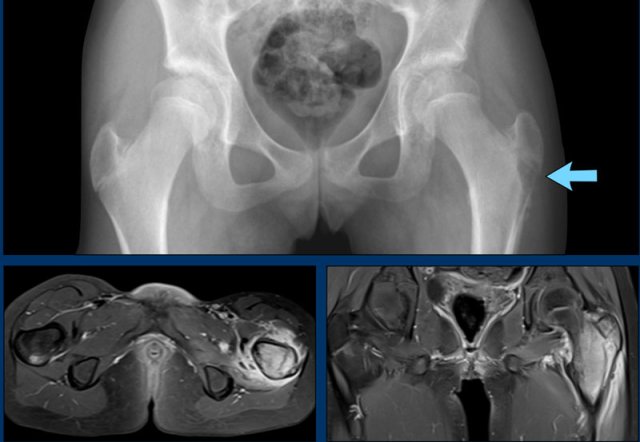
This radiograph of the pelvis is of a patient with tuberculous arthritis of the left hip joint.
There is subtle joint space narrowing with some subchondral sclerosis of the left hip.
These radiographic findings are nonspecific and most likely would be the result of osteoarthritis..
Continue with the MRI...
Much to everyone's surprise there were multiple abscesses.
When abscess formation is this extensive and the clinical findings are minimal, always think of tuberculous arthritis.
The diagnosis of tuberculous arthritis was made by joint aspiration.
Spondyloarthritis - SpA
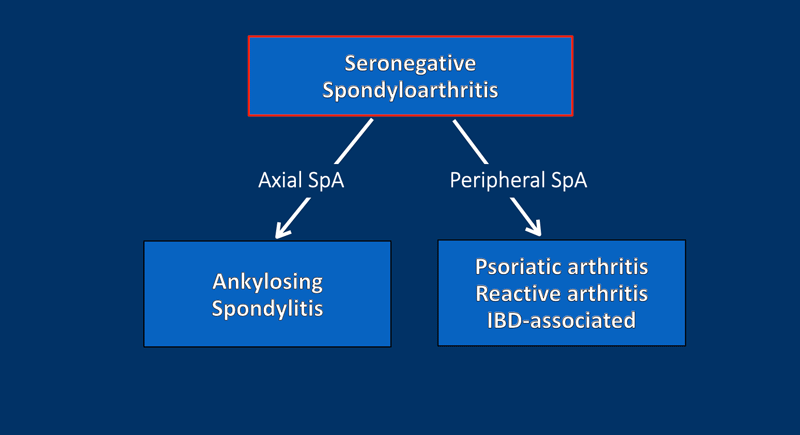
Spondyloarthritis (SpA) comprises a group of inflammatory diseases of the joints and spine, with various clinical manifestations.
There have some key features in common, including:
- joint inflammation, especially SI joints
- enthesitis, especially of the lumbar spine
- HLA-B27 genetic factor association
- Rheumatoid factor negative (seronegative)
Spondyloarthritis can further be divided into an axial and a peripheral type.
Ankylosing spondylitis is the most common axial type and the prototypical type of spondyloarthritis.
The most common peripheral types are psoriatic arthritis, reactive arthritis and enteropathic arthritis (associated with inflammatory bowel diseases).
Classification criteria for SpA from the Assessment of SpondyloArthritis International Society (ASAS) are:
- ≥3 months of back pain and age of onset ≤ 45 years
- and sacroiliitis on imaging plus ≥1 clinical feature
- or HLA-B27+ plus 2 other clinical features
The clinical features of spondyloarthritis are listed in the table.
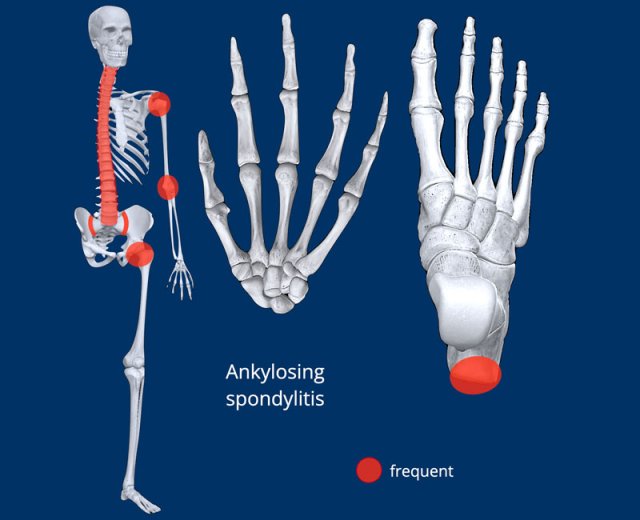
Ankylosing Spondylitis
Key findings
Axial arthropathy, with enthesitis (edema, shiny corners), syndesmophytes and sacro-iliitis.
Clinical
Significant back pain, morning stiffness and disability.
The onset is in the 3rd and 4th decade and the prevalence is about 1%.
Ankylosing Spondylitis is the prototypical type of seronegative, axial SpA and primarily affects the spine and SI-joints although other joints like shoulders, hips, ribs, heels and small joints of the hands and feet can become involved.
Radiological
- Shiny corners of vertebral bodies
- Bamboo spine
- Sacro-iliitis
Enthesitis
Inflammation of the enthesis is one of the hallmarks of SpA.
The earliest sign of ankylosing spondylitis is edema at the enthesis, which is only visible on MRI (white arrow).
In a later stage sclerosis will present as shiny corners on X-rays or CT.
Finally syndesmophytes are formed along these enthesis (see next images).
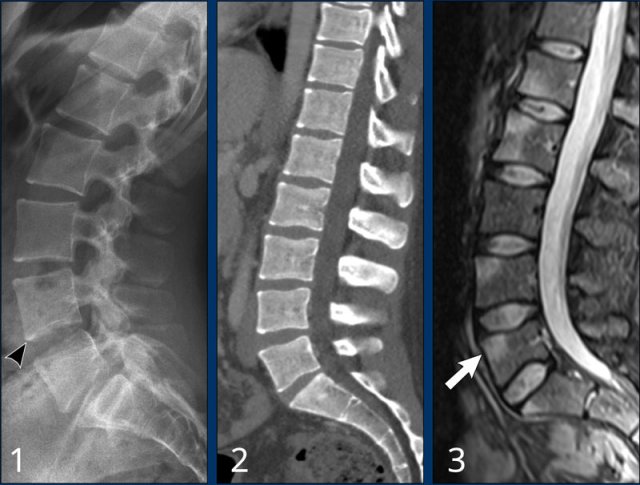
Images
Three different patients with typical features of early stage ankylosing spondylitis:
- Shiny corners of the anterior border of vertebrae where the enthesis is located. Squaring of the vertebral bodies is seen.
- Another patient with squaring and shiny corners of the vertebral bodies on CT.
- This patient has edema at the enthesis of vertebral bodies, visible on sag STIR.
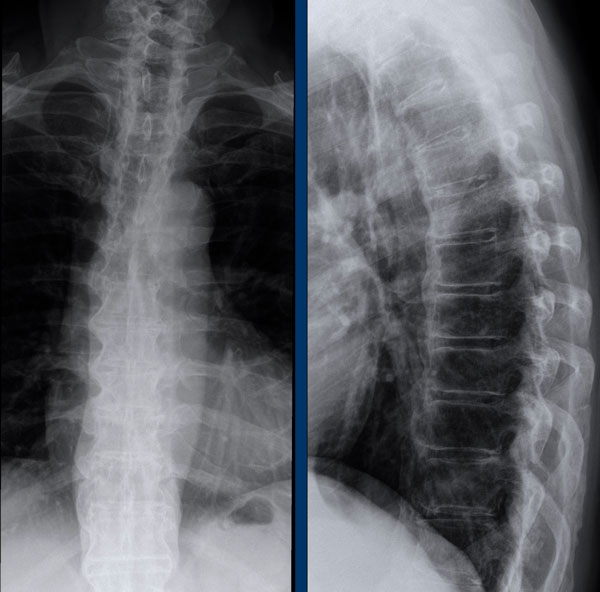
Syndesmophytes
These images show syndesmophytes in the lumbar spine and ossification of the paraspinal ligaments.
When these syndesmophytes fuse, this produces the typical “bamboo spine” appearance.
Also note the ossification of the intervertebral disc and ankylosis of the facet joints.
Syndesmophytes have a typically vertical orientation.
Bridging and fusing is quite common.
As a result the spine looses its flexibility and can easily fracture even after a minor trauma.
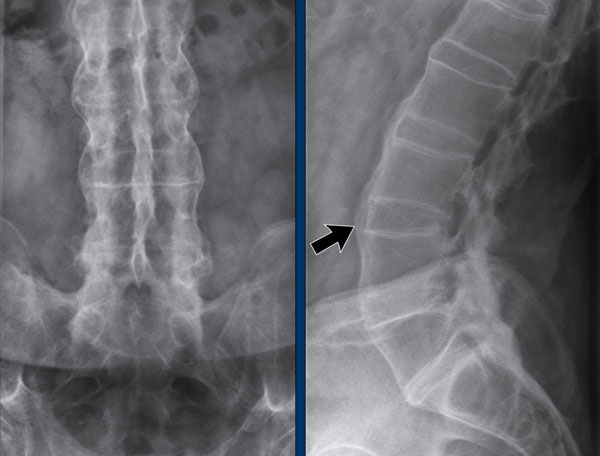
Bamboo spine
Bamboo spine in ankylosing spondylitis.
Fusion of the lumbar spine by syndesmophytes and ossification of the paraspinal ligaments.
Notice the ligamentous calcification (arrow).
A rigid bamboo spine is prone to hyperextension fractures, even after mild trauma.
Always have a high suspicion of these fractures in a rigid spine!
A bamboo spine often begins at the lumbar level and can ascend up to the cervical spine.
Notice the squaring of the vertebral bodies (arrow).
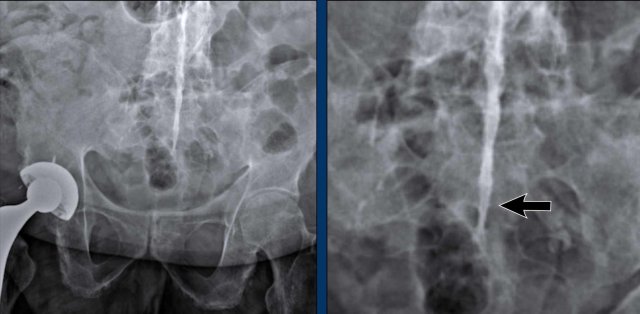
Dagger sign
The radiopaque central line on frontal radiographs of the spine due to ossification of the interspinous ligaments, known as the “dagger sign”, is a radiographic feature of ankylosing spondylitis.
Also note the complete fusion of the SI-joints.
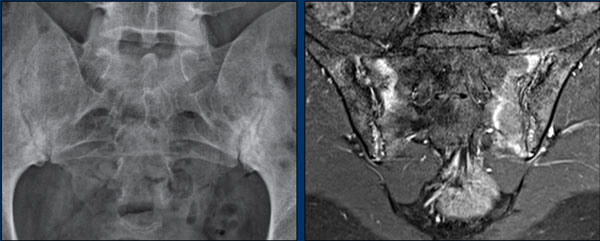
Sacro-iliitis
An important hallmark of SpA is sacro-iliitis.
It starts with inflammation, which is visible on MRI as edema, with or without erosions (visible on MRI and conventional imaging).
Later on you will see fatty metaplasia on MRI or sclerosis alongside the SI-joints on radiographs.
In the end stage there is ankylosis of the SI-joints.
X-ray
Bilateral subchondral sclerosis and erosions of the sacroiliac (SI) joints caused by sacro-iliitis.
MRI
T1W post contrast MR of the same patient shows an irregular contour of the SI-joints caused by erosions.
There is enhancement in the subchondral bone and bone marrow edema.
There is no joint effusion.
I.V. contrast does not necessarily have to be used for the diagnosis of sacro-iliitis.
Scroll through the MR-images and compare with the findings on the X-ray (last image).
Differential Diagnosis of sacro-iliitis:
- Osteoarthritis: bilateral subchondral sclerosis without erosions of the SI-joints.
- Osteitis condensans Ilii: bilateral triangular shaped sclerosis of the ilium adjacent to the SI-joint.
The diagnosis of sacro-iliitis can be challenging based on these X rays alone. It can be helpful to include an X-LWK or other investigation to become more certain.
Late stage sacro-iliitis with ankylosis of the SI-joints.
Hatchet sign versus avascular necrosis
The hatchet sign differs from the deformity seen in avascular necrosis, where there is progressive collapse of the articular surface of the humeral head.
Milwaukee shoulder
A rare shoulder arthropathy that can simulate the hatchet shoulder is the Milwaukee shoulder syndrome.
It is characterized by rupture of the rotator cuff and large joint and bursal effusions with deposition of hydroxyapatite crystals leading to rapid destruction of the glenohumeral joint.
Image
Severe destruction of the humeral head with cephalic migration and erosions of the acromion indicating total cuff rupture.
In the Milwaukee shoulder syndrome, symptoms are often much milder than imaging suggests.
In this case, there was no attempt to diagnose calcium hydroxyapatite crystals in the synovium.
Based on clinical and radiographic findings, Milwaukee shoulder syndrome was diagnosed.
Ankylosis of the hip joints with joint space narrowing in a patient with ankylosing spondylitis.
There is also ankylosis of the sacroiliac joints.
Psoriatic arthritis
Key findings
Erosions and bone proliferation predominantly in a distal distribution, presenting most often as a typical pathognomonical pattern, but sometimes as a confusing subtype (see differential diagnosis).
Clinical
Psoriatic arthritis is a peripheral type of spondyloarthritis and presents as a peripheral arthritis with or without sacroiliitis and spondylitis.
It frequently is preceded by psoriasis of the skin, but can occur without skin disease in up to 20% of patients.
Enthesopathy is common.
The hands are most commonly involved followed by the feet. Other locations are the spine, sacroiliac joints and less frequently knee, elbow, ankle and shoulder.
Radiological findings
- Articular: small marginal bone erosions, arthritis mutilans with acro-osteolysis and pencil-in-cup deformities, joint subluxation, interphalangeal ankylosis, sacroiliitis (frequently asymmetrical).
- Bone: bone productive changes, periostitis, Ivory phalanx (distal phalanx dig 1), spondylitis (asymmetrical paravertebral ossifications).
- Cartilage: joint space narrowing
- Distribution: see illustration, asymmetric and predominantly peripheral.
- Extra findings: skin lesions, telescoping fingers.
- Soft tissue: Enthesitis, dactylitis (sausage digit), onycholysis (the nail separates from the skin).
Differential Diagnosis
Rheumatoid arthritis, erosive osteoarthritis, reactive arthritis
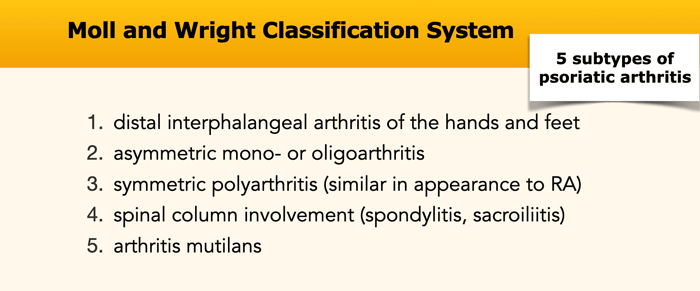
There are five subtypes of psoriatic arthritis.
Due to these different patterns, the diagnosis of psoriatic arthritis can sometimes be challenging.
Sausage digits
Typical appearance of dactylitis “sausage digits” with soft tissue swelling and pencil-in-cup deformity of DIP 1-2 and 5 of the left hand in a patient with psoriatc arthritis.
Notice that the MCP joints are not involved (unlike in RA).
Progressive psoriatic arthritis
- The picture on the left shows marginal erosions (black arrow) and subtle bone formation (blue arrow) of the IP joint.
- Later on, it progresses to the typical pencil-in-cup deformation.
The distribution and the bone formation makes the diagnosis of rheumatoid arthritis unlikely.
The marginal erosions and the absence of DIP involvement in other joints makes the diagnosis of erosive osteoarthritis unlikely, although pencil-in-cup can look like the gullwing deformity in erosive osteoarthritis.
Pencil in cup deformity
A. Pencil in cup deformity of 1st and 5th toe.
B. Acro-osteolysis with resorption of the terminal tuft of digits 2-4 and 5.
There are erosions in MTP 2 and 3.
Periostitis in psoriatic arthritis
This is a patient with psoriatic arthritis.
Notice the subtle periostitis of the distal phalanx of dig 1 on the right (arrowhead).
There are small erosions of the tuft of dig 2 and 3 on the left (white arrows).
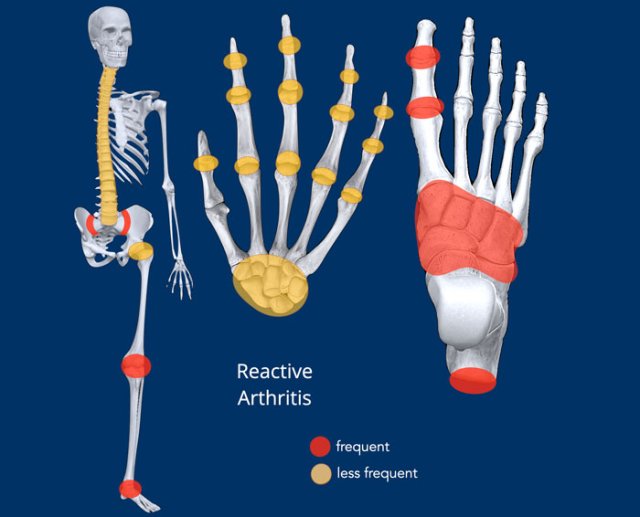
Reactive arthritis
Clinical
Reactive arthritis is a sterile arthritis following soon after an infection
elsewhere in the body, usually of genitourinary or enteric origin.
It is caused
by a cross-reaction of the antigen reaction to bacteria as well as synovial
tissue.
Classically patients present with conjunctivitis and urethritis,
leading to the triad: can't see, can't pee and can't bend the knee.
Radiological findings
- Articular: in later disease ill-defined erosions like psoriatic arthritis (typically calcaneus is involved)
- Bone: Bone proliferation but also juxta-articular osteoporosis and enthesopathy/enthesitis
- Cartilage: uniform joint space narrowing.
- Distribution: asymmetric, see illustration
- Extra findings: usually triggered by a preceding infection
- Soft tissue: swelling soft tissue (also sausage digit)
This patient suffered from an episode of campylobacter gastroenteritis.
After a
few weeks clinical symptoms of arthritis emerged.
Image
On the right there are
erosions at the base of the 3rd proximal phalanx and at the head of the 5th
proximal phalanx (white arrowheads).
On the left there is an erosion at the base of the 3rd proximal
phalanx and lytic changes of the head of the 1st proximal phalanx (yellow arrowheads).
Based on the aspecific imaging findings alone, it is difficult to diagnose reactive arthritis.
The preceding infection makes it more likely.
Diffuse Idiopathic Skeletal Hyperostosis
Key findings
Bulky spondylophytes, over more than 4 contiguous levels, located at the right side of the lower thoracic vertebrae.
Clinical
Diffuse Idiopathic Skeletal Hyperostosis (DISH) is also known as Forestier’s disease. Most often asymptomatic.
It is characterized by bony proliferation at tendinous and ligamentous insertion of the spine and pelvis mostly affecting elderly individuals.
Radiological findings
- Articular: no erosions
- Bone: Calcification or ossification of the
anterior longitudinal ligament, paraspinal connective tissue and annulus
fibrosis over a region of at least four contiguous vertebral bodies. These are of typical 'bulky' appearance.
Usually they are located on the right side, since pulsations of the aorta prevent spondylophytes from forming. - Enthesopathy of the pelvis (e.g. iliac crest, ischial tuberosities, greater trochanters)
- Cartilage: Typically preservation of disc height without profound degenerative disc disease.
- Distribution: The lower thoracic spine is most frequently affected. Usually there is no involvement of synovial lower part of the sacroiliac joint, although ossification of ligamentous upper part of the SI joint can occur.
- Extra findings: Prone to severe fracture after minor trauma.
- Soft tissue: increased susceptibility to fractures
Teaching point
In daily practice, it is the classic differential diagnosis of ankylosing spondylitis, especially in early stages of both diseases.
Teach yourself the differences between the two (see below).
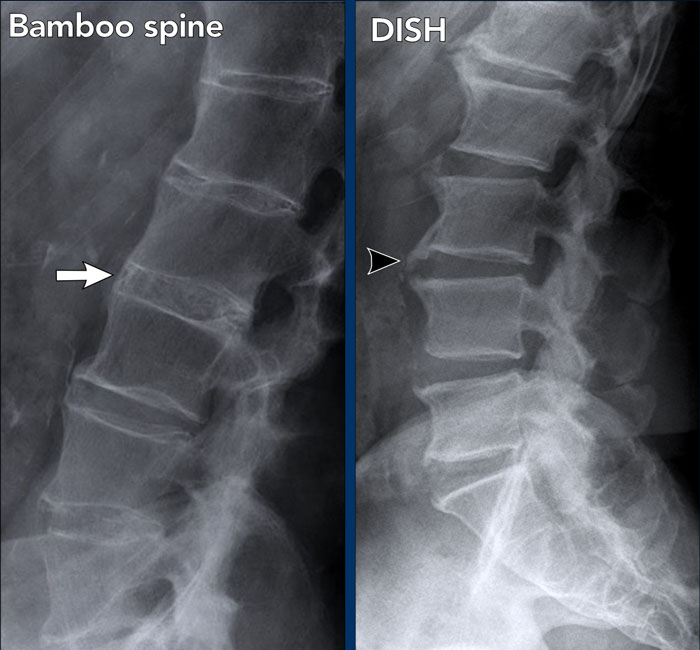
DISH should not be confused with the findings of a bamboo spine, which is the hallmark of ankylosing spondylitis.
Image
- Bamboo spine: fusion of the lumbar spine by subtle syndesmophytes and ossification of the paraspinal ligaments.
- DISH: bulky ossification and calcification of the anterior longitudinal ligament and the paraspinal connective
tissue over more than 4 contiguous levels. Typically preservation of disc
height without profound degenerative disc disease.
Other causes of ligamentous ossification in the spine are severe osteoarthritis, and less likely: vitamin A toxicity and fluorosis.
Image of another patient with DISH.
There is enthesopathy of the iliac crest, ischial tuberosities and greater
trochanters.
The lower part of the SI joint is normal (unlike ankylosing spondylitis).
Ossification of the ligaments in the upper part of the SI joint is present.
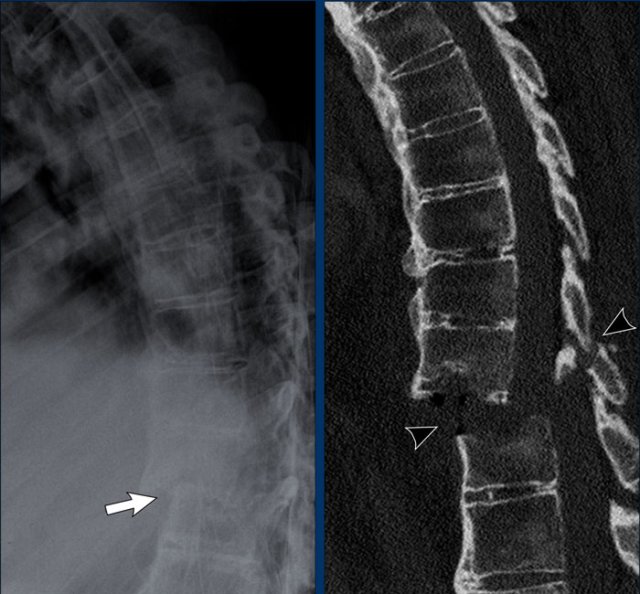
Image
Typical ossification and calcification of the anterior and paraspinal ligament
and connective tissue over more than 4 contiguous levels.
Large
ossifications of the anterior longitudinal ligament.
There is some non-typical
narrowing of facet joints.
No sign of
degenerative disc disease.
Ankylosis due to DISH and ankylosing spondylitis can result in a rigid spinal column. Then, the spine is prone to fracture after even mild trivial trauma. These fractures are most often hyperextension fractures.
This patient had a minor trauma, which however resulted in an unstable hyperextension fracture with neurological complications.
Teaching point: you should always have a high suspicion of hyperextension fractures in patients with rigid spine due to DISH and ankylosing spondylitis.
Gout
Key findings
Tophi with juxtaarticular erosions at the capsule insertion of a joint, typically MTP1, in patients with risk factors like diabetes and kidney disease
Clinical
Gout
is an inflammatory arthropathy caused by the deposition of sodium urate
crystals in joints and periarticular soft tissues and tendons. The first MTP
joint is most often affected (podagra). Classically the diagnosis is made
clinically, supported by joint aspiration.
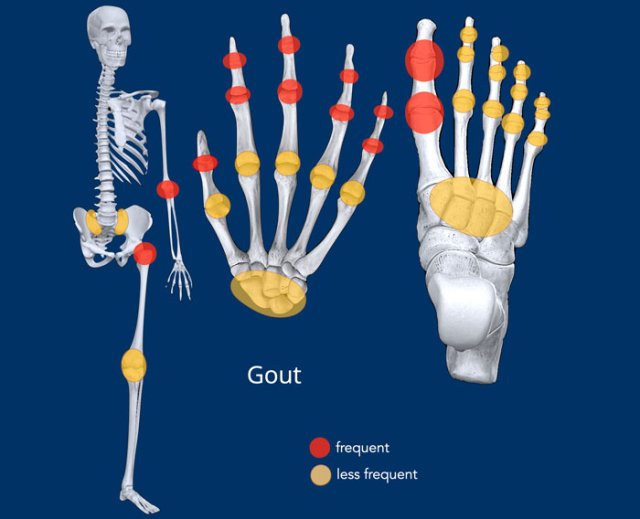
Radiological findings
- Articular: “punched out “ erosions >5 mm, that spare part of the joint with an overhanging edge of new bone.
- Bone: bone mineralization is normal. Chondrocalcinosis or osteonecrosis can occur.
- Cartilage: joint effusion (earliest sign), preservation of joint space
- Distribution: see illustration, there is a predilection for peripheral joints. Most often it has an asymmetric, random distribution.
- Extra findings: usually male, hyperuricemia
- Soft tissue: tophi: pathognomonic, eccentric nodular soft tissue swelling due to crystal deposition around the joints is common. These may be hyperdens due to the crystals and may calcify. Olecranon and prepatellar bursitis.
Late stage of Gout
Characteristic radiologic changes in the
chronic stage of gout.
Typically well-defined “punched-out” eccentric erosions with sclerotic margins in a marginal and juxta-articular distribution.
These erosions have overhanging edges called rat bite erosions.
There is preservation of joint spaces.
Periarticular hyperdense soft tissue swelling due to tophi as a result of crystal depositions (pathognomonic).
These are located in the ligamentous structures around the joints.
Typical involvement of the 1st MTP joint with punched-out erosion.
The soft tissue swelling represents a tophus.
The dislocation is not a common finding in gout, but in this case the result of the erosions and ligamentous injury.
Soft tissue density
Typical dense soft tissue swelling surrounding the 1st MTP joints bilateral.
Juxta-articular erosions at the medial side of the distal MT, which have sclerotic margins.
They are most notably on the right side (arrow).
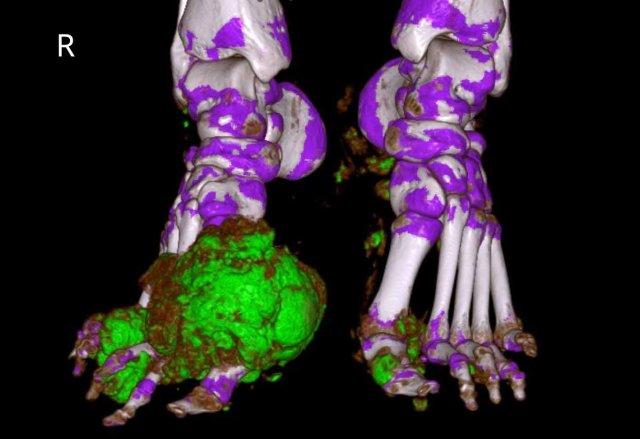
Continue with the Dual Energy CT...
Dual Energy CT of the same patient with gout showing the urate crystal depositions.
In
this 3D reconstruction the crystal depositions are color coded green and can be
seen surrounding the MTP joints and at the insertion of the right achilles
tendon (arrow).
The green pixels in the nail beds of digitus 1 and 5 on the left are artifacts caused by keratin in thickened nails.
Dual
Energy CT is a noninvasive method of urate crystal detection that can
make joint aspiration unnecessary.
Dual Energy CT simultaneously scans the subject at two different energy levels.
Because urate crystals show different attenuation at these energy levels, the
crystals can easily be identified with high accuracy.
Another case with typical gout tophi and juxtaarticular erosions on plain films.
Dual Energy CT shows gout attenuation in MTP1, MTP2 and interphalangeal joints of the 3rd digit.
DECT is useful for the diagnosis when findings are not so typical.
It is also very useful to show the extent of disease.
In this case, a bone tumor was suspected.
There are definitely some findings that could support the diagnosis of an osteosarcoma of chondrosarcoma.
However, this was proven to be gout.
Continue with the DECT images...
With these DECT images, nobody was in doubt anymore.
Punched out erosions
In this case there is a classical punched out erosion of the MCP3 joint with an overhanging edge (arrow).
The borders of the erosions in gout can be sclerotic because of the indolence of the process, creating a punched-out or “mouse bitten” appearance.
Calcified tophi
The images show extensive tophi around the knee joint in a patient with gout (arrowheads).
In the knee, these locations (insertion popliteus tendon, insertion quadriceps tendon, insertion MCL) are very typical.
There is mild
joint effusion.
The joint space narrowing is likely due to secondary
osteoarthritis.
When in doubt, think gout
This is a difficult case.
Small bilateral erosions of the PIP
joints on both sides are seen.
The arrowheads show that the erosions are more juxtaarticular in this patient that proved to have gout.
Based on the distribution, rheumatoid arthritis and psoriatic arthritis would have been an option.
However then the erosions would have been more marginally located.
Also, the MCPs are spared, making the diagnosis of rheumatoid arthritis less likely.
Soft tissue swelling
This case is also challenging.
Multipele joint are affected, but there is no typical distribution.
The only thing that these joints have in common is the surrounding hyperdense soft tissue swelling.
This was due to gout tophi.
CPPD
Key findings
Fine chondrocalcinosis located at the TFCC or menisceal tissue in the knee.
Clinical
Calcium Pyrophosphate Deposition (CPPD) is an inflammatory joint disease caused by deposition of calcium
pyrophosphate dihydrate crystals into the synovial fluid, synovial lining and
articular cartilage.
Some terms regarding CPPD can be a bit confusing:
- Chondrocalcinosis
Descriptive term when fine calcifications in cartilage are present, most often used when CPPD is the cause. However, chondrocalcinosis is not an exclusive feature of CPPD and can also be seen in severe osteoarthritis.
Most patients are clinically asymptomatic. - Pyrophosphate arthropathy
Distinctive arthropathy of CPPD, which is similar to osteoarthritis, but with a funny distribution.
There is chondrocalcinosis and large chondral cysts, that can simulate a osteolytic neoplasm. - Pseudogout
Acute joint inflammation due to CPPD. It is called pseudogout because clinically it can look like gout.
Radiological findings
- Articular: no erosions
- Bone: subcortical cyst formation
- Cartilage: joint space narrowing
- Distribution: see illustration, symmetrical.
- Extra findings: no
- Soft tissue: chondrocalcinosis, especially along the cartilage. The TFCC and knee joints are preferred spots.
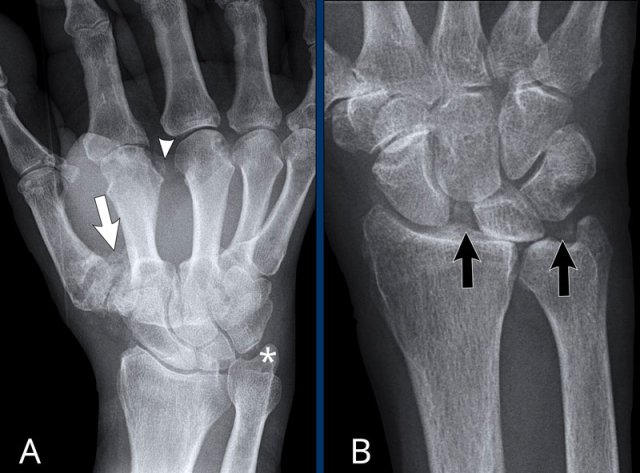
Two patients with typical CPPD.
A. There is cartilage loss in many joints and chondrocalcinosis in:
- CMC1 (white arrow)
- MCP joints (arrowhead)
- TFCC (asterix)
B. This patient had an acute joint inflammation. Chondrocalcinosis in the radiocarpal joint and the TFCC (black arrows) is seen, almost pathognomonical for CPPD. There is scapholunate dissociation, which can be seen in CPPD, but also in rheumatoid arthritis or posttraumatic.
This sudden attack is called pseudogout, because it can simulate the inflammation and intense pain of a gout attack.
Chondrocalcinosis in CPPD
There
are faint calcifications of the cartilage and meniscus both on the right side
(white arrow) as well as on the left side (black arrows).
These can be caused
by CPPD, but may be seen in other conditions as well, such as gout or
osteoarthritis.
Also note the joint space narrowing and mild osteophyte
formation.
CPPD has many features similar to osteoarthritis.
There is a well-circumscribed coarse calcification adjacent to the 4th DIP joint. This does not look like CPPD and scleroderma would have been more likely.
However, aspiration revealed typical CPPD crystal depositions.
As in other arthropathies, atypical presentations of CPPD are possible, but fortunately less common.
Scleroderma
Key findings
Soft tissue calcifications and acro-osteolysis
Clinical
Scleroderma (systemic sclerosis) is an autoimmune connective tissue disease and
is characterized by microvascular obliteration and sclerosis of the skin and
internal organs.
The
clinical hallmark of the disease is the appearance of taut tethering of the
skin.
Clinically evident arthritis occurs in up to 65% of patients, and it may
be one of the earliest manifestations of scleroderma.
There
is a limited and a multisystem variant.
CREST syndrome is a common type of limited scleroderma (skin calcinosis,
Raynaud’s phenomenon, esophageal dysmotility, sclerodactyly
and telangiectasia).
The systemic variant can affect virtually every organ system or can be
localized.
Radiological findings
- Articular: erosions, pencil-in-cup deformity, resorption of the 1st CMC joint with radial subluxation.
- Bone: acral osteolysis (resorption of the distal phalanges), periarticular osteopenia.
- Cartilage: joint space narrowing
- Distribution: see illustration, symmetric
- Extra findings: scleroderma has a lot of other organ manifestations like pulmonary and abdominal organ manifestations.
- Soft tissue: skin thickening, cutaneous calcifications (often at mechanically exposed locations), acral soft tissue necrosis.
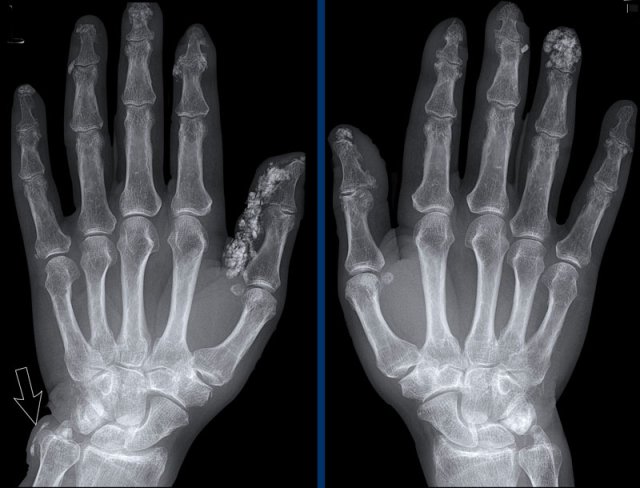
Soft tissue calcifications
Extensive soft tissue calcifications in the distal phalanges in a patient with scleroderma.
Notice the calcifications next to the distal ulna (arrow).
There are no signs of cartilage damage.
The pathophysiology of the calcium deposits is not well
understood.
It occurs in tissues that are under chronic stress, such as local
trauma or damage associated with an underlying inflammatory process.
It is usually
more abundant in the dominant hand.
When these findings are present, the diagnosis is usually straight forward.
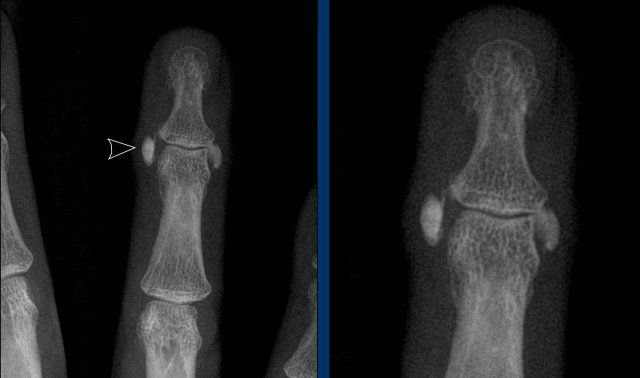
Subtle, but coarse soft tissue calcifications at the most distal part of the finger in a patient with scleroderma.
No acro-osteolysis or other signs are seen.
Acro-osteolysis in Scleroderma
Severe acro-osteolysis of the finger tips of dig 1-3 in a patient with scleroderma (arrows). Notice the lysis of the soft tissues distally.
Acro-osteolysis is a
radiographic finding which refers to bone destruction of the distal phalanges and occurs in 6–65% of patients with scleroderma.
Vascular alterations and
reduced capillary density impair tissue oxygenation and the resulting hypoxia
may contribute to osteoclast activation.
There is a wide variety of diseases that can cause acro-osteolysis including psoriatic arthritis, infection, raynaud disease and thermal trauma.
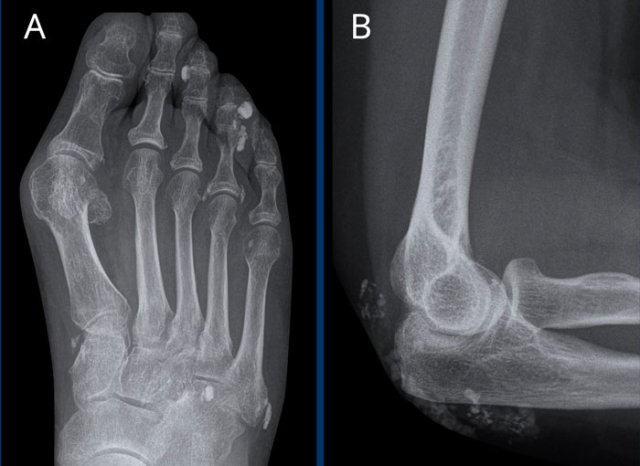
A. Subcutaneous and periarticular calcifications in the foot of a patient with scleroderma.
There is also a hallux valgus deformity, which is not caused by scleroderma.
B. Subcutaneous calcifications near the elbow in a patient with scleroderma.
These subcutaneous calcifications often form at pressure points.
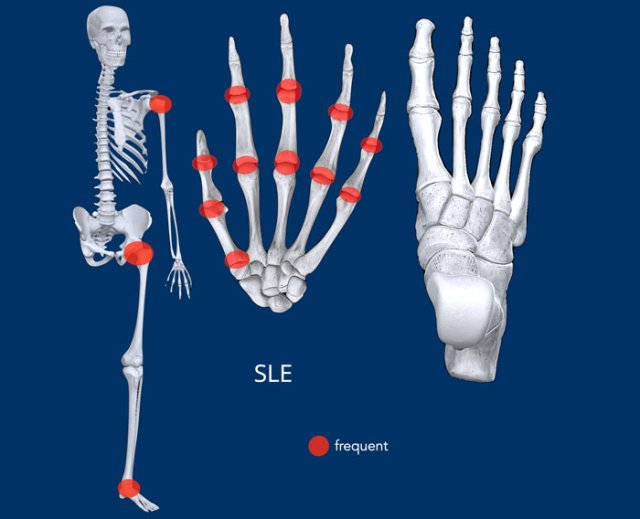
Systemic lupus erythematosus
Key findings
Abnormal joint alignment without erosions. Avascular necrosis.
Clinical
SLE is a generalized autoimmune connective tissue disease.
Essentially any
organ system can be affected with systemic (weakness, malaise, fever),
mucocutaneous (typical butterfly rash on the face), renal and neurological
symptoms.
Radiological findings
- Articular: no erosions
- Bone: periarticular osteoporosis
- Cartilage: normal joint spaces
- Distribution: see illustration, symmetric distribution
- Extra findings: avascular necrosis
- Soft tissue: reducible deformities like swan neck and boutonniere deformities. Soft tissue swelling. Calcifications in the subcutaneous and deep soft tissues may be seen, most often around small joints.
Z-thumbs and swan neck fingers in a patient with SLE.
The deformities are
thought to be a consequence of low-grade inflammation of the synovial membrane
and capsule resulting in ligamentous laxity and muscular contracture.
Swan neck deformity
Here another example with extensive alignment deformities without erosions or signs of cartilage damage in a patient with SLE.
Another patient with a swan
neck deformity.
Usually this is reversible in the early stage of the disease.
Avascular necrosis
Avascular
necrosis is a frequent complication in SLE in up to 15% of patients.
The femoral
head and tibial plateau are the most involved sites, but other sites may be
affected.
SLE patients with bone pain should be suspect of having
avascular necrosis.
Avascular necrosis in SLE can occur even in the
absence of steroid use.
Images
Increased density in the distal femur in a guirlande-like pattern, representing avascular necrosis in a
patient with SLE.
A. Subluxation of the 1st MCP joint without erosions in a patient with SLE. This is not typical for SLE and can be seen in other forms of arthritis like for instance osteoarthritis.
B. SLE of the shoulder. Collapse of the humeral head with some loose bony fragments due to avascular necrosis. Both steroid therapy and SLE are associated with an increased risk of avascular necrosis.
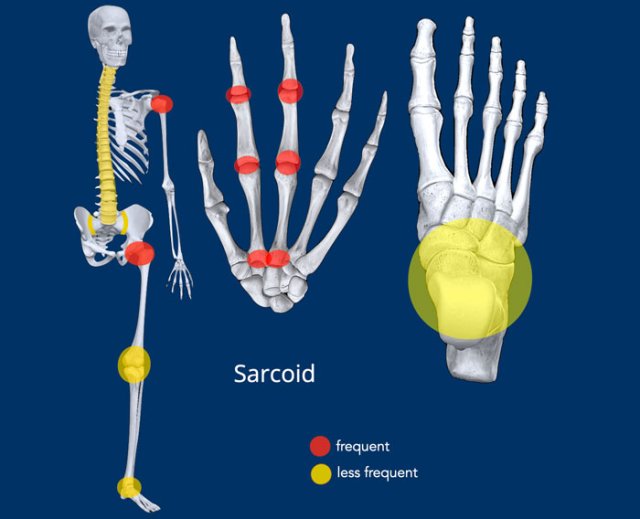
Sarcoid
Key findings
Lace-like granuloma lesions in the bone
Clinical
Sarcoidosis is a multisystem disorder of unknown etiology characterized by
the formation of inflammatory non-caseating granulomas.
Musculoskeletal manifestations of
sarcoidosis occur in about 20% of patients with sarcoidosis and include joint
involvement, bone lesions, and muscular disease.
Primary skeletal involvement
without other organ involvement is extremely rare. Usually arthritis is seen
early in the course of sarcoid disease, chronic sarcoid arthritis is rare.
The most frequent musculoskeletal
manifestation of sarcoidosis is an acute arthritis that occurs as part of
Löfgren’s syndrome characterized by the combination of erythema nodosum,
bilateral hilar adenopathy, polyarthritis, and constitutional symptoms.
Radiological findings
- Articular: erosions
- Bone: sarcoid bone lesions can be permeative or “moth-eaten”, lytic or sclerotic. These lesions are very distinctive.
- Cartilage: joint space narrowing is unusual.
- Distribution: Typically there is multiple joint involvement with symmetric distribution, see illustration.
- Extra findings: There are a wide range of manifestations and thereby also many clinical and radiographic manifestations.
- Soft tissue: dactylitis, myopathy.
Lace-like granulomas
Multiple bone lesions in a patient with sarcoid.
The osteolytic lesions are quite typical and described as having a lace-like or trabecular pattern.
Once you have seen this, you will recognize it in other cases.
The image shows an osteolytic lesion in the distal radius (blue arrow) with trabecular and cortical bone destruction in a patient with sarcoid.
There is osseous destruction on both sides of the interphalangeal joint of the first digit with extraosseous extension of granulomatous tissue (black arrow).
Amyloidosis
Clinical
Amyloidosis is a systemic disease in which normally soluble proteins
(amyloid) are deposited as an insoluble proteinaceous material in the
extracellular spaces.
Amyloid is often deposited into the heart, kidney, gastrointestinal tract and
nervous systems.
The secondary form of amyloidosis is associated with diseases such as multiple myeloma, hemodialysis, RA and chronic infection.
Musculoskeletal manifestations are most often depositions in periarticular tendons and capsule.
Amyloid arthropathy is extremely rare and only 5-13% of patients have bone or joint involvement.
Radiological findings
- Articular: erosions in a late stage of disease
- Bone: subchondral cysts
- Cartilage: joint space widening in early stages due to intra-articular amyloid deposition
- Distribution: symmetric, in shoulders and wrist.
- Extra findings:
- Soft tissue: purulent synovial fluid and bulky soft tissue nodules
Amyloidosis is very difficult to diagnose on conventional imaging alone, MR is more useful for the diagnosis.
T2W series of a patient with amyloid arthropathy of the shoulder joint.
The findings are:
- Large intra-articular swelling caused by the deposition of hypointens amyloid.
- Spread to the subacromial and subscapular space.
- Large erosions of the humeral head.
This
soft tissue swelling should not be mistaken for rice bodies as seen in rheumatoid
arthritis.
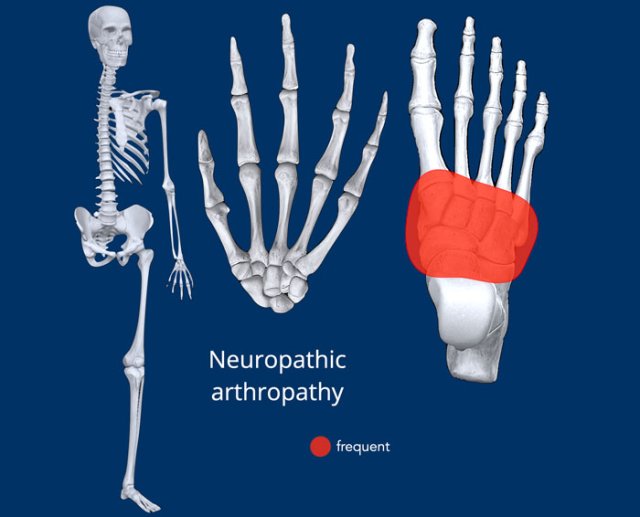
Neuropathic arthropathy
Clinical
Neuropathic arthropathy also known as Charcot arthropathy is a progressive destructive joint disorder in patients with peripheral neuropathy with
loss of pain sensation and proprioception in the foot, ankle or hands.
Patients may experience fractures and dislocations of bones and joints with
minimal or no known trauma.
The most common cause is diabetes mellitus, which typically affects the tarsal
and tarso-metatarsal joints. Arterial wall calcification is commonly seen in
these patients. Other causes are tabes dorsalis
(tertiary syphilis), syringomyelia, leprosy and CPPD.
Radiological findings
- Articular: no erosios
- Bone: early phase consists of inflammation and osteopenia. Finally joint destruction with loose bodies, fragmentation and insufficiency fractures. When Charcot is treated and becomes less active, bone will coalescense with formation of osteophytes and bony proliferations.
- Cartilage: joint space narrowing and ankylosis
- Distribution: frequently asymmetric.
- Extra findings: neuropathy and vasculopathy.
- Soft tissue: soft tissue swelling. Severe joint malalignment leading to rocker-bottem deformity.
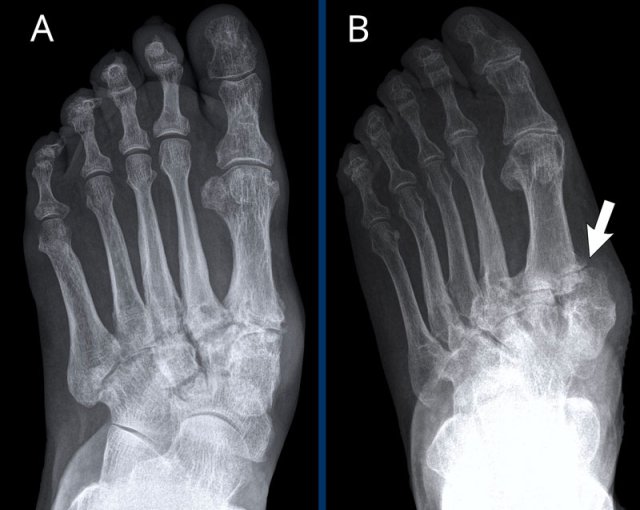
These radiographs are of two different patients with diabetes and neuropathic arthropathy.
A. Destruction of the tarsometatarsal joints with periarticular lucencies.
B. Typical
radiological changes in the foot of a diabetic patient. There is lateral
subluxation of the TMT joints (Lisfranc dislocation).
The changes in bone and joints itself may mimic severe osteoarthritis, severe inflammation or septic arthritis.
The key in this case is the clinical history with the presence of diabetic neuropathy.
Rocker bottom deformity
On this weight-bearing lateral view the dislocation in the TMT joints is even better visible.
For a more detailed explanation of diabetes-related foot problems go to MRI examination of the diabetic foot.
Diabetic Hand Syndrome
The diabetic hand syndrome is the inability to use the hand due to contractures and stiffness.
It can affect the
proximal and distal IP and MCP-joints and
is often painless.
Prolonged hyperglycemia is thought to result in the accumulation of advanced
glycation end products (AGEs).
These AGEs can break down collagen and
deposit abnormal amounts of collagen in connective tissue around the joints,
resulting in stiffening and hardening of the joints and the skin.
Images
Destruction of the CMC-1 and all DIP-joints.
Erosions and bone destruction adjacent to the IP1, DIP 2-5 and PIP 4-5.
There is subluxation of PIP 4-5 and DIP 2-5.
Notice the extensive vascular calcifications in a patient with
Diabetes Mellitus type 2.
The hand of this patient with neuropathy shows a status after removal of the trapezium (arrow).
There is destruction of all DIP joints and erosions adjacent to the PIP and MCP joints.
There are erosions and bone destruction adjacent to the IP1, the DIP and PIP and MCP joints.
There is subluxation and dislocation of DIP 2, 4 and 5 and PIP 2-4.
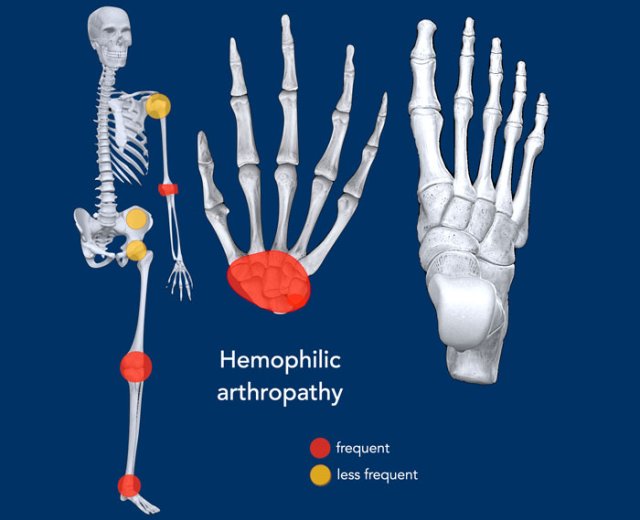
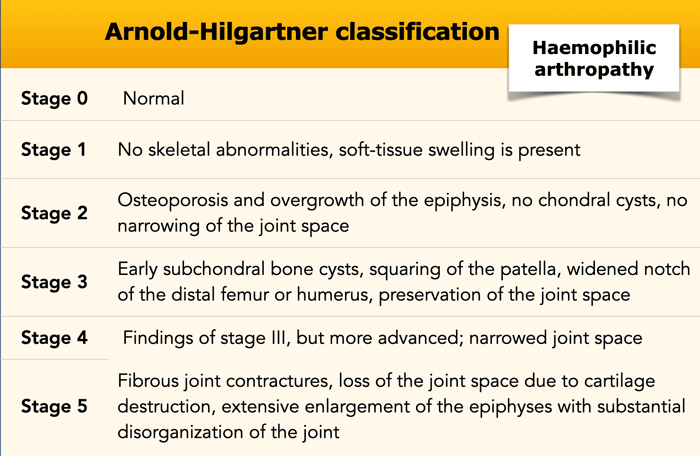
Hemophilic arthropathy
Key findings
Extensive findings that look like osteoarthritis, but in an unusual distribution or pattern.
Clinical
Hemophilia is an inherited coagulation bleeding disorder which is mainly
X-linked recessive and therefore occurs almost exclusively in males.
About 50% of the hemophilia patients develop haemophilic arthropathy.
This results from recurrent hemarthrosis, which leads to synovial hyperplasia, chronic inflammation, fibrosis, and
hemosiderosis.
It is frequently mono- or oligoarticular.
Early prophylaxis with coagulation factors considerably reduces the musculoskeletal complications.
Radiological findings
- Articular: erosions and eventually joint destruction
- Bone: subchondral bone cyst formation, osteoporosis (mostly periarticular due to hyperemia), ankylosis in late stage
- Cartilage: joint space narrowing and destruction in late stage of disease
- Distribution: hemarthrosis affects large joints and is frequently mono- or oligoarticular, see illustration
- Extra findings: growth abnormalities
- Soft tissue: soft tissue swelling due to joint swelling or extra-articular hemorrhage.
Teaching point: when findings look like osteoarthritis, but in an odd presentation or distribution, think hemophilic arthropathy.
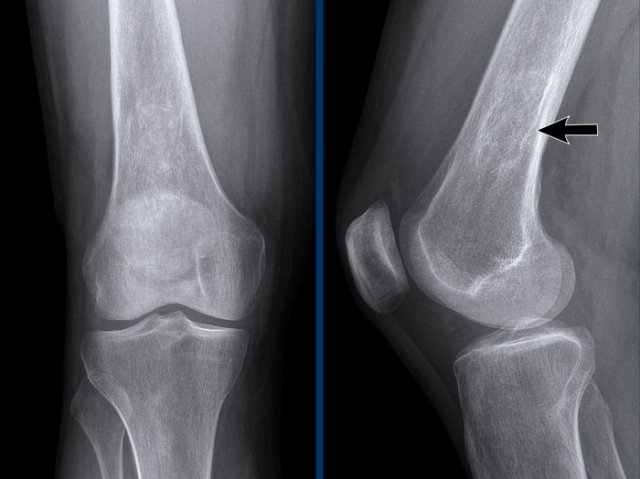
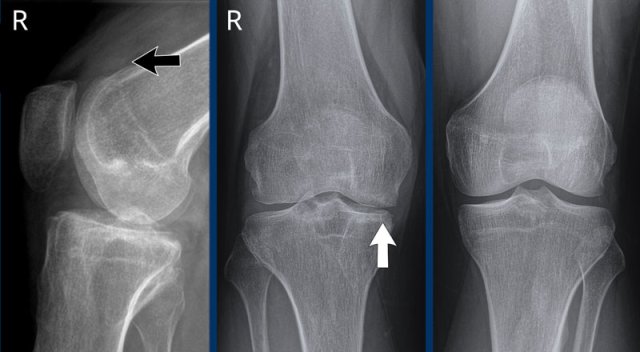
This patient has a history of hemophilia and repetitive hemarthros.
Images
Distention
of the suprapatellar recess of the right knee due to hemarthrosis (black arrow).
There is narrowing of the medial joint space
caused by cartilage destruction and secondary osteoarthritis (white arrow).
Subchondral bone
cyst formation underneath the intercondylar eminence.
No erosions.
This patient has a history of repetitive hemarthrosis caused by a vascular malformation (not visible on plain radiography).
Images
The image of the right knee shows joint space narrowing, subchondral cysts formation and
erosions of the medial and lateral tibial plateau.
Normal left knee joint for comparison.
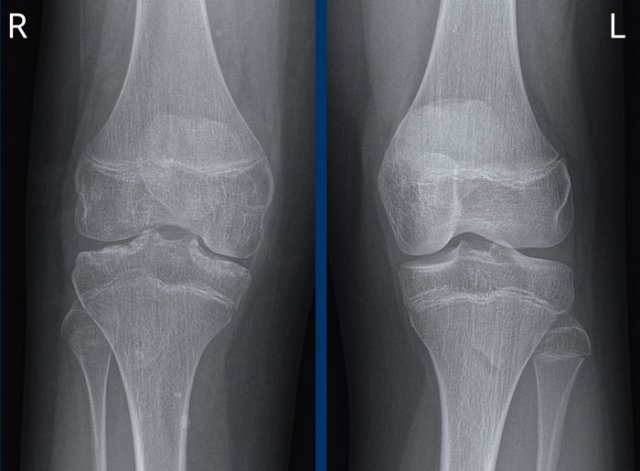
This patient has a long term history of repetitive hemarthrosis as a result of hemophilia.
Images
A slightly widened intercondylar notch on the left hand side, which can also be
found in juvenile rheumatoid arthritis and tuberculous arthropathy.
Bulbous
femoral condyles with flattened condylar surfaces.
The congruent bony
deformation on the left hand side can also be seen in tuberculous arthropathy.
This is stage V Arnold-Hilgartner classification hemophilic arthropathy. with severe joint space narrowing, subchondral cyst formation and erosive destruction.
This image is of a patient with hemophilia and recurrent hemarthrosis of the shoulder joint.
There are features of secondary osteoarthritis with subchondral sclerosis and
osteophyte formation at both sides of the glenohumeral joint.
In general
hemophilic arthropathy has similarities with osteoarthritis.
However, the
presence of erosions, extensive subchondral bone cyst formation and the history of recurrent hemarthrosis are distinguishing features in favor of hemophilic arthropathy.
Image of the ankle of a patient with hemophilia.
The findings are:
- extensive symmetrical joint space loss,
- subchondral bone cyst formation
- erosive changes
End Stage hemophilic arthropathy
The findings are:
- symmetric joint space narrowing
- joint effusion
- subchondral cyst formation
- secondary osteoarthritis with osteophytes
Although the findings itself are not that specific, you can see the resemblance between all of the above cases.
CRMO - chronic recurrent multifocal osteomyelitis
Key findings
Multifocal areas of sterile bone inflammation
Clinical
Chronic Recurrent Multifocal
Osteomyelitis (CRMO) is an uncommon autoinflammatory disorder of the bone of children
and young adults that is characterized by nonbacterial osteomyelitis.
Patients present with
episodic multifocal bone pain secondary to sterile osseous inflammation. The disease has a relapsing and remitting course. The cause of CRMO is
unclear. The diagnosis is made by exclusion, and the main causes to be excluded
are neoplasms and infections.
It is sometimes diagnosed along with inflammatory
bowel disease or psoriasis and there seems to be a genetic component.
CRMO is
comparable to SAPHO in adults.
Radiological findings
- Articular: no abnormal findings.
- Bone: first lytic lesions and bone edema, later progressive sclerotic lesions in metaphysis. Also periostitis.
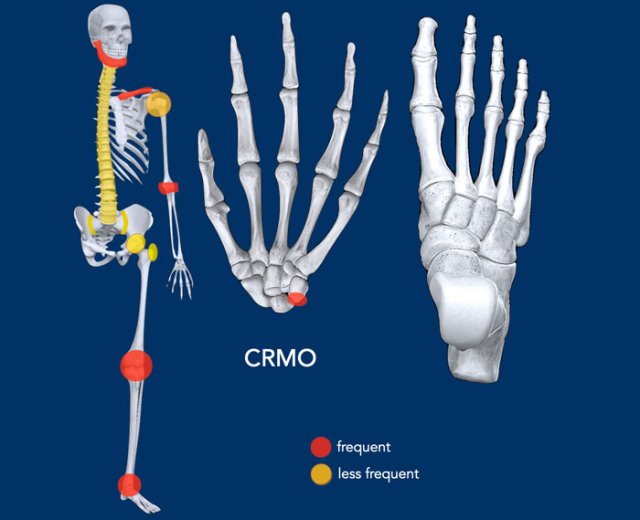
- Cartilage: no abnormal findings
- Distribution: see illustration, often symmetrical and multifocal. Typically medial clavicles and tibia are involved. Other common sites are rib, mandible, pelvis and vertebral bodies.
- Extra findings: occurs in children and adolescents with an average age of onset of 7-14 and a female to male ratio of approximately 2:1.
- Soft tissue: edema in soft tissue around the CRMO.
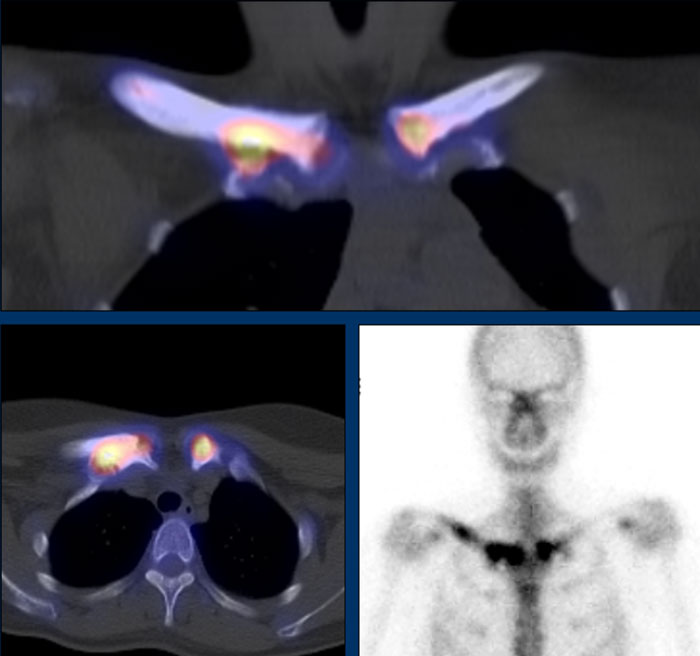
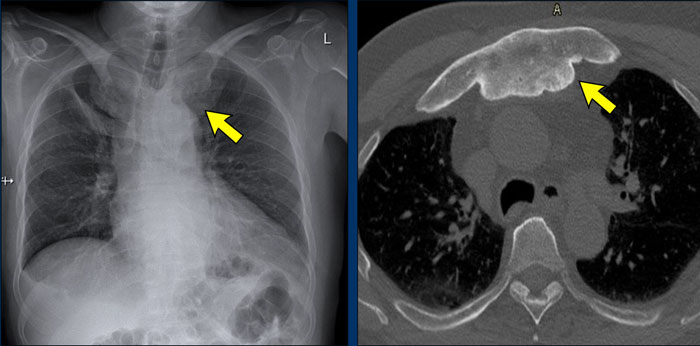
Cortical thickening, sclerosis and bone enlargement of the diaphysis and metaphysis of the right clavicle and the metaphysis of the left clavicle.
SPECT-CT and Bone scintigraphy of the same patient. Abnormal tracer uptake in corresponding areas, reflecting increased bone turnover.
X-ray of a patient with CRMO with pain on the left side.
There is subcortical osteolysis lateral in the proximal femur (arrow)
The MRI (axial and coronal T1 TSE FS with contrast) shows a region of bone and soft tissue enhancement.
This was due to non-infectious
osteomyelitis with extra
osseous extension.
There is also a small CRMO location visible in the dorsal aspect of the trochanter major on the right.
Multiple CRMO locations
This patient has locations in the humeral head and proximal diaphysis and in the coracoid on the right and the distal tibia on both sides.
SAPHO syndrome
Clinical
SAPHO syndrome (synovitis, acne, pustulosis, hyperostosis, and osteitis)
is an uncommon inflammatory disorder of bone, joints and skin.
The pathogenesis of SAPHO syndrome is not
well understood.
It is sometimes described as an autoinflammatory disorder.
The
pediatric counterpart of the disease is known as CRMO.
Radiological findings
- Articular: joint erosions and erosion at the vertebral body corners.
- Bone:
Osteitis (bone inflammation), seen as sclerosis of the medullary cavity and bone marrow edema.
Hyperostosis (excessive bone growth), seen as cortical thickening, formation of osteophytes, paravertebral ossification and ankylosis.
Osteolysis is also a common finding and may lead to vertebral body collapse. - Cartilage: joint space narrowing is present
- Distribution: asymmetric, anterior chest wall is the most common site of involvement, see illustration.
- Extra findings: Usually seen in an average age of 30 to 50 years with a female predominance.
- Soft tissue: Acne and pustulosis of palms and soles, although skin and osteoarticular manifestations do not necessarily coexist.
Teaching point: the degree of inflammation determines the type of bone abnormalities. Osteolysis will occur when there is extensive inflammation. Increase of bone activity and sclerosis will occur when there is less inflammation.
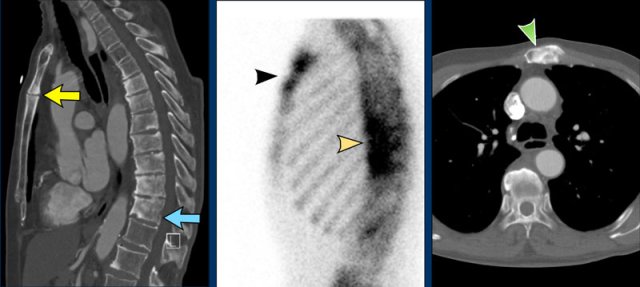
Patient with SAPHO syndrome with:
- osteïtis of corpus and manubrium sterni and sclerotic thoracic vertebral bodies, some endplate erosions and paravertebral syndesmophyte formation (left, sag CT)
- increased bone turonver (middle, bone scintigraphy)
- sclerosis in manubrium sterni (right, axial CT)
Hyperostosis in SAPHO
This patient has extensive hyperostosis of the medial side
of the clavicles on both sides.
CT of the same patient.
There is
extensive hyperostosis of the medial side of the clavicles and sternum.
Ankylosis of the sternoclavicular and of the first and
second sternocostal joints.
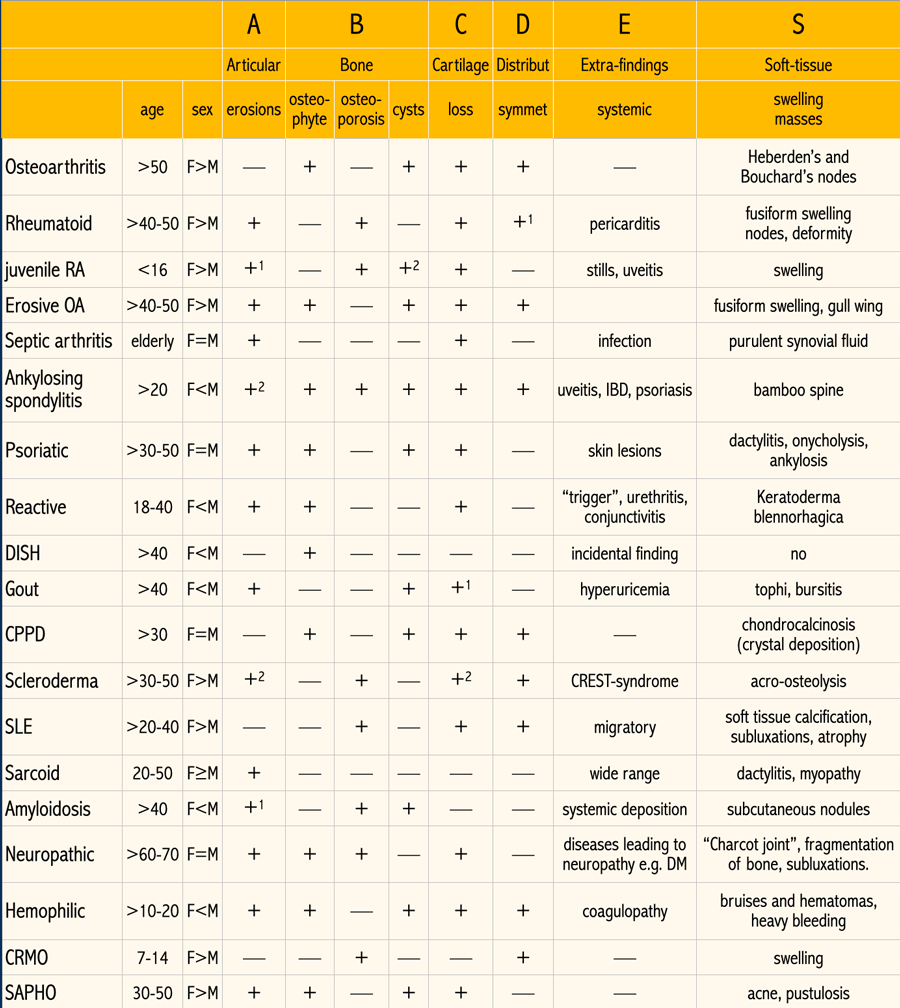
ABCDE-S overview
In this table the key findings of the various joint diseases are summarized according to the ABCDE-S mnemonic.
Click on the image for a larger view.